Dev Cell:周俊等解析肿瘤微环境对肿瘤生长的影响
2021-07-03 小柯生命 小柯生命
2021年6月30日,德国癌症研究中心和海德堡大学 Michael Boutros 课题组在 Developmental Cell 期刊在线发表了题为:Microenvironmental innat
组织发育是通过细胞对局部环境的适应来实现的。组织发育同时需要动态的细胞重排,包括竞争和消除一个细胞群体来扩展一个更具竞争力的细胞群体。因此动物组织内细胞的存活和生长会受到‘细胞竞争’的影响。这种细胞竞争现象最初是在果蝇组织中的正常细胞与失去生长优势的突变细胞之间发现的。
不同细胞群之间的动态相互作用直接或间接地促进了组织内有限的资源和空间的竞争。肿瘤的生长同样也利用这种机制来消灭其周围的细胞以利于自身的生长。然而,肿瘤如何消除其微环境中的正常细胞的相关分子机制尚不清楚。
2021年6月30日,德国癌症研究中心和海德堡大学 Michael Boutros 课题组在 Developmental Cell 期刊在线发表了题为:Microenvironmental innate immune signaling and cell mechanical responses promote tumor growth 的研究论文。
该研究利用组织特异性CRISPR基因敲除技术生成BMP信号通路突变体,建立了一个诱导型果蝇肠道肿瘤模型,来研究肿瘤微环境对肿瘤生长的影响。
该项研究解析了肿瘤微环境中先天免疫信号通路以及肿瘤对周围正常细胞形成的机械细胞竞争压力影响肿瘤生长的分子机制。
德国癌症研究中心周俊博士为论文第一作者和共同通讯作者,德国癌症研究中心和海德堡大学Michael Boutros教授为论文最后通讯作者。
在肿瘤生长初期,这种细胞自我扩张的机制对于肿瘤的生长和发展起着至关重要的作用。因此,研究肿瘤如何在致密的组织中生长的机制则变得非常重要。这些机制可以让我们了解和检测癌症发展的早期阶段,并为制定更好的治疗癌症的策略提供理论依据。
肿瘤微环境中先天性免疫的激活刺激肿瘤生长
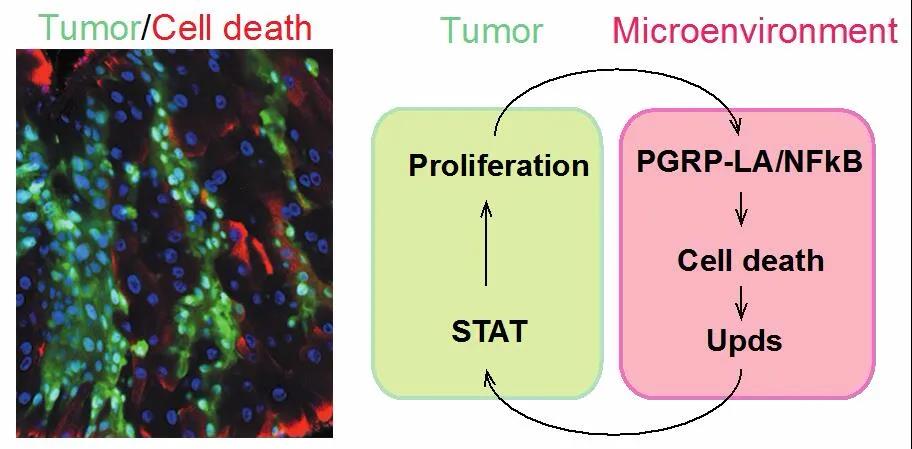
研究团队首先通过对肠道肿瘤和正常组织的基因表达图谱分析,发现肿瘤中与先天性免疫反应相关的基因的表达水平明显上升。同时他们发现先天性免疫激活主要在肿瘤周围的正常细胞中(肿瘤微环境)。
进一步的研究发现,携带肿瘤的肠道中先天性免疫(NFκB)信号通路的激活需要上游受体 PGRP-LA。这一系列PGRP-LA/NFkB信号通路激活可以诱导肿瘤微环境中正常细胞的凋亡。
同时,凋亡的细胞能分泌细胞因子Unpaired(Upd)来激活肿瘤细胞中JAK/STAT信号通路的活性从而促进肿瘤生长。研究人员随后发现遗传缺失NFkB 活性及其上游调节分子 PGRP-LA 能够降低肿瘤微环境中的细胞凋亡以及抑制肿瘤的生长。
肿瘤微环境中先天性免疫系统激活对肿瘤生长的影响
肿瘤通过机械细胞竞争压力消除周围正常细胞
动物在发育过程中会消除一些不合适的细胞来维持自身组织健康。组织稳态失衡时,例如在肿瘤生长过程中,这种竞争性生长的分子机制还并不十分清楚。因此,研究团队假设肿瘤细胞由于生长优势挤压周围的正常细胞并诱导竞争性细胞凋亡来实现肿瘤细胞扩张。接下来,研究团队通过细胞机械传感器 (Mechano-Sensor)监测细胞骨架变化和胞间连接张力来研究肿瘤微环境中的分子变化。
他们发现肿瘤生长会在其微环境中诱导 Rho 相关蛋白激酶(ROCK)/JNK 相关的细胞机械力反应。施用 ROCK 抑制剂可挽救与肿瘤相关的细胞机械力反应,并引起肿瘤的肠道中胁迫、免疫和凋亡相关基因的表达水平下降。此外,ROCK 抑制剂的处理能有效的限制肿瘤生长。
总的来说,该研究发现肿瘤细胞通过机械性竞争压力排挤周围正常细胞,从而激活免疫应答的NFkB通路,诱导周围正常细胞分离和凋亡,从而促进肿瘤生长。这个过程需要激活机械力响应相关的ROCK/JNK信号通路通过调控上游肽聚糖识别蛋白PGRP-LA来完成。
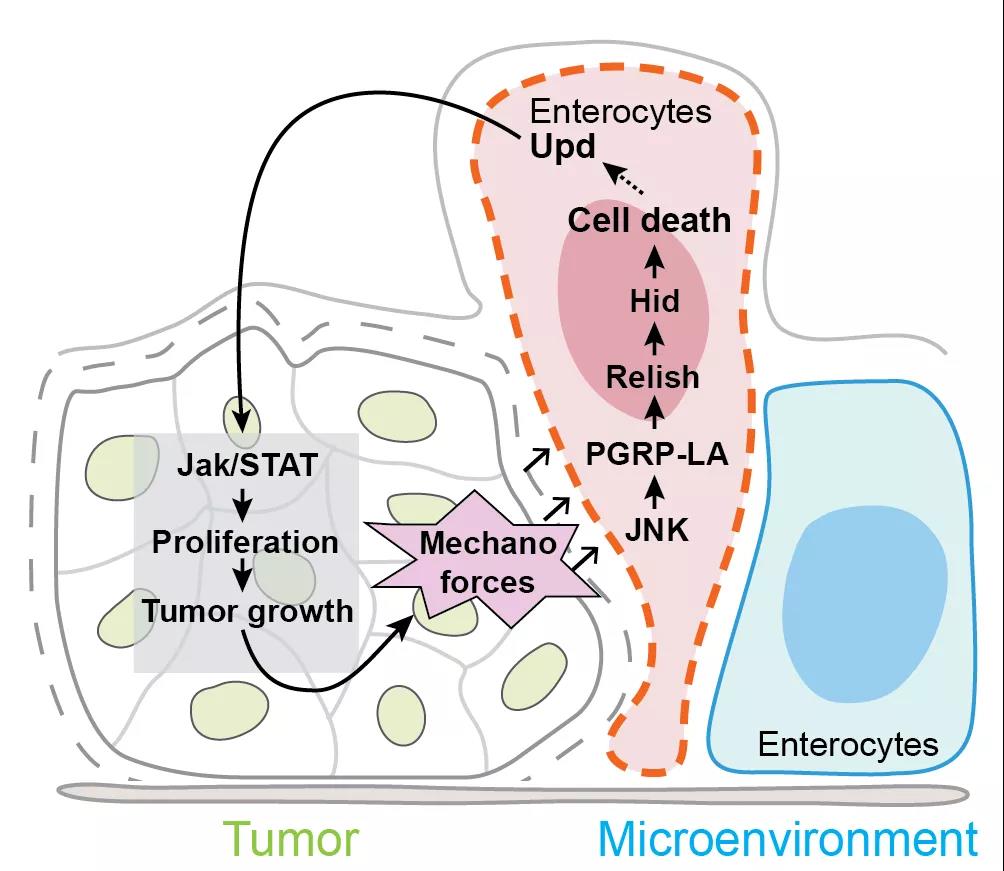
肿瘤微环境中机械性竞争引起炎症性细胞凋亡的模型
本研究首次阐明了肿瘤通过“劫持”一种炎症反馈机制,通过机械性细胞竞争来消除肿瘤周边的肠上皮细胞,从而支持自身生长。另一项最新的独立研究在人肾脏上皮细胞模型中也发现并证实了免疫应答的NFκB通路参与调控感染过程中利用机械应力消除被感染细胞的一种免疫保护机制。
原始出处:
Jun Zhou, et al. Microenvironmental innate immune signaling and cell mechanical responses promote tumor growth. Developmental Cell, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肿瘤微环境#是一个热点问题,未来需要攻克其治疗#靶点#
94
#Dev#
47
#解析#
35
#CEL#
41
#Cell#
42