Nat Commun:恶性胸膜间皮瘤的克隆结构可作为预后指标并影响肿瘤微环境
2021-03-24 xiaozeng MedSci原创
恶性胸膜间皮瘤(MPM)是一种罕见的、无法治愈的癌症。
恶性胸膜间皮瘤(MPM)是一种罕见的、无法治愈的癌症。其发病率在全球范围内仍在不断增长。全球每年的发病率为每百万人7至40例,而每年约有38,400例死亡病例。
MPM通常在接触石棉后20–50年被诊断出,且其正沿着未知的进化轨迹发展。在过去的二十年中,这一普遍致死的癌症仅出现了十分有限的药物开发,且缺乏个性化的治疗方法。
为了阐明MPM中的基因组内肿瘤异质性(ITH),研究人员对手术中获得的来自22例MPM患者的90个肿瘤样品进行了多区域外显子组测序。
MPM的基因组肿瘤内异质性
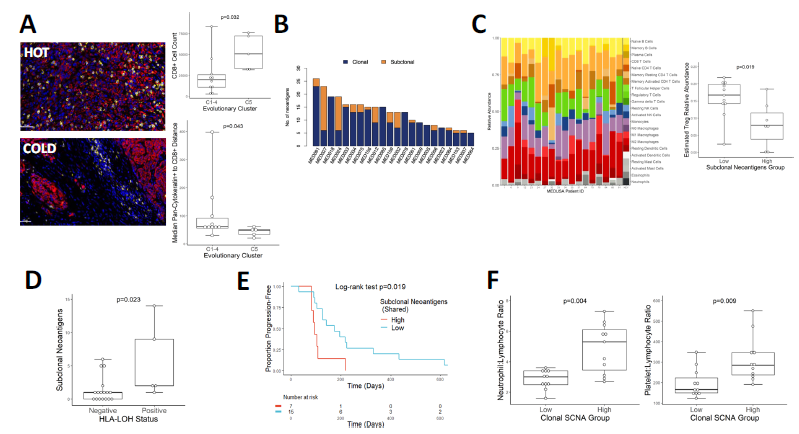
研究人员发现,在整个队列中外源性肿瘤内异质性差异很大。系统进化树模型反映了基因组不稳定的陡峭梯度。通过迁移学习模型,研究人员检测到了重复进化,并解析了5个可预测的聚类。
克隆结构塑造了MPM的免疫微环境
BAP1/-3p21和FBXW7/-chr4事件始终发生于早期克隆。相反的,导致Hippo通路失活的NF2/-22q事件则主要发生于克隆晚期,而在亚克隆中则表现出了平行进化,表明进化受到了限制。在术后12年,有一名患者发生了非常晚期的体细胞NF2/22q改变。克隆结构和进化簇决定了MPM的炎症反应和免疫逃逸。
总而言之,该研究结果揭示了MPM中潜在的可成药的进化瓶颈,以及克隆结构对免疫格局塑造的影响,并可能决定了对免疫检查点抑制作用的临床反应。
原始出处:
Zhang, M., Luo, JL., Sun, Q. et al. Clonal architecture in mesothelioma is prognostic and shapes the tumour microenvironment. Nat Commun 12, 1751 (19 March 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#胸膜间皮瘤#与#肿瘤微环境#
74
#克隆#
38
#胸膜#
27
#COMMUN#
27
#Nat#
39
#预后指标#
45
#间皮瘤#
36
Mpm
64
肿瘤微环境。
75
没有几分真难受
72