心率增快是高血压常见的一种临床表型。法国 10万人群的调研发现,未治疗的高血压患者平均心 率较正常血压者增快6次/min。2014年,我国21个 城市115 229例高血压患者的横断面调查显示,我 国高血压患者的静息平均心率为76.6次/min,单纯 高血压患者中心率≥ 80次/min者占38.2%。这与 意大利的一项研究结果相似,后者显示高血压患者 中30%以上静息心率≥ 80次/min。近年来,高血 压伴心率增快患者的心率管理问题逐渐受到重视, 因为在不同人群中进行的诸多流行病学研究显示, 心率增快很可能是一项重要的心血管危险因素,可 增加心血管事件和死亡风险。
pixabay
2017年我国发表《高血压患者心率管理中国专 家共识》,专家们针对心率增快是否导致靶器官损 害、如何界定心率增快等问题逐个进行讨论,提出了针对我国高血压患者心率管理的共识性建议。 最近3年中,在心率检测技术、心率增快机制以及心率增快的不利后果等方面均有较多新的、重要的 研究结果发表,尤其是我国学者的大样本研究弥补 了国内既往循证资料的不足。此外,越来越多的研究发现,心率增快的不利影响还涉及与高血压 密切相关的多种内分泌、肾脏和神经内科疾病,心率管理需要多学科临床医生的参与。因此,我们决定撰写《中国高血压患者心率管理多学科专家共识 (2021年版)》。
1.高血压患者心率测量
心率测量方法:心率可通过脉搏触诊、心脏听诊、电子血压计、心电图、动态心电图或动态血 压等进行测量。心律失常尤其心房颤动时,脉搏触 诊、电子血压计或动态血压测量均可能造成误差, 因此,推荐通过心脏听诊计数心率。心房颤动患者 的心脏听诊时间应持续至少1 min。
诊室心率:通过脉搏触诊、心脏听诊计数心 率。影响心率的因素包括生理因素、心理因素、环 境和体位等。

家庭自测心率:家庭自测心率与诊室心率和 24 h平均心率的相关性良好。建议患者在使用家庭 自动血压计测量血压的同时记录心率,尽可能在清 晨安静状态下自测心率。
动态心率监测:可通过24 h动态心电图和动 态血压测量获得。与诊室心率相比,动态心率能为 临床提供更多有价值的信息,包括心率的昼夜节律 变化、心率变异性、夜间心率和避免白大衣效应。
2. 心率增快的原因和机制
生理性:生理性窦性心动过速较常见,运动、 体位改变、焦虑、情绪激动、妊娠、饮酒、饮用咖 啡、饮茶、吸烟等均可使心率增快。
药物性:阿托品、苯丙胺等副交感神经阻断 药物,肾上腺素、麻黄素等拟交感神经药物,丙米嗪、 阿米替林等三环类抗抑郁药,以及左西孟旦、米力农、氨茶碱、短效硝苯地平,或突然停用β受体阻 滞剂等均可引起心率增快。
病理性:贫血、疼痛、感染、发热、甲状腺 功能亢进、低血糖、嗜铬细胞瘤、低血压、休克、 肺栓塞、慢性阻塞性肺疾病、多种心血管疾病如急 性心肌梗死、心力衰竭、心肌炎、心包炎或心肌病 等均可引起心动过速。
心率增快与心血管事件相关的病理机制:流行病学显示的心率与心血管事件的相关性,在进行临 床验证之前,首先要有发病机制方面的合理解释。
3. 高血压患者需要心率管理的证据
尽管迄今为止尚缺乏前瞻性以心率作为干预靶 点对临床终点影响的药物试验,也缺乏高质量的前 瞻性随机对照试验证实减慢心率本身即能带来显著 的临床获益,但从流行病学角度来看,心率增快可视为一项独立的心血管危险因素。因此,对心率增快的高血压患者予以适当的药物干预是合理的。

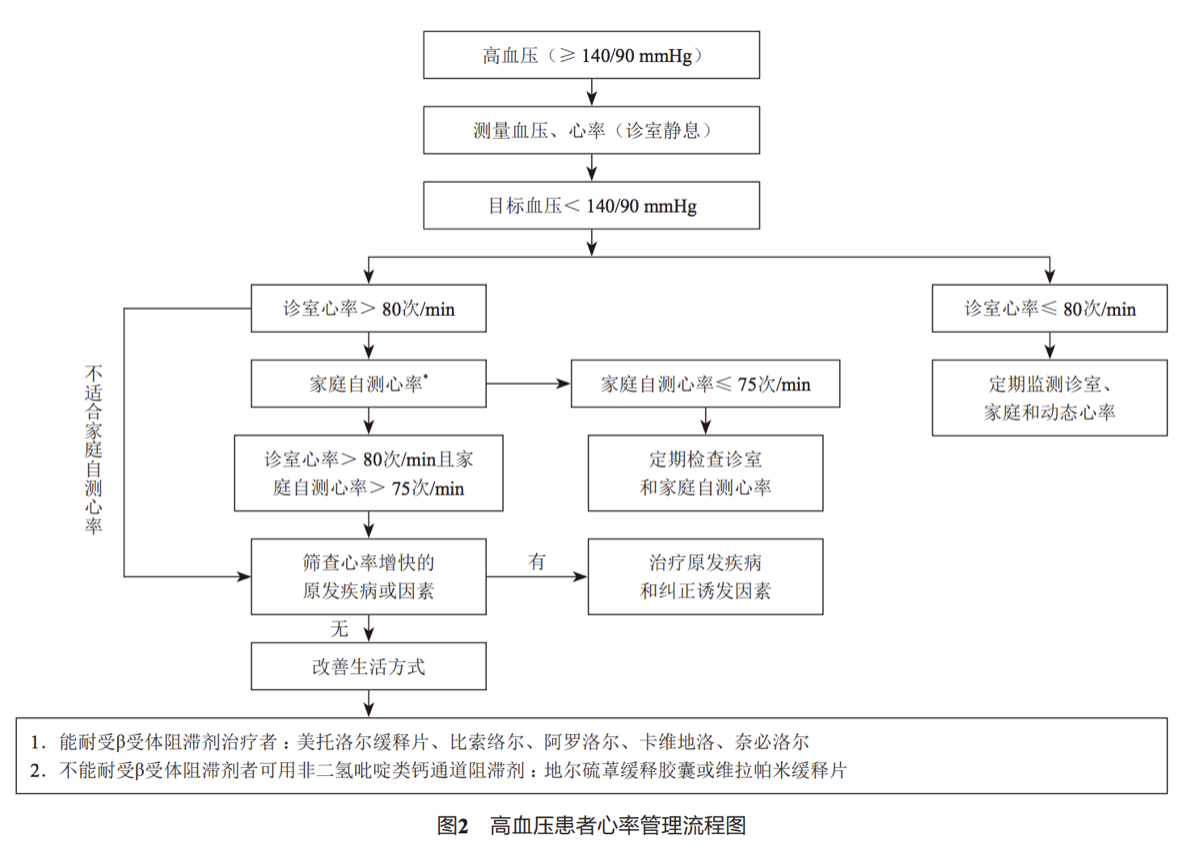
4. 高血压患者心率干预的切点
传统上正常窦性心律的定义为60 ~ 100次/min。但这一定义只是早年专家们的一种共识,没有经过任何科学验证。欧洲高血压学会专家组认为,根据现有的流行 病学数据,高血压患者和普通人群的心率干预切点 为80 ~ 85次/min。本共识专家组综合分析现有循 证医学证据,参考欧洲高血压学会的意见,建议将 我国高血压患者的心率干预切点定义为静息心率> 80次/min。本共识还建议,高血压患者在静息状态 下不同时间点的多次家庭自测心率均> 75次/min, 也可视为心率增快。
5. 高血压患者心率管理的干预方法
(1)首先应排查高血压患者心率增快的诱因和 原因,包括生理性、药物性、心血管疾病或全身性 疾病(见前述),对此应针对影响因素及原发疾病 予以纠正和治疗。
(2)对高血压伴心率增快患者,需改善不良的生活方式,如久坐、高盐饮食、吸烟、酗酒,大量 饮用咖啡和浓茶会促进交感神经兴奋而使心率增 快。
(3)高血压伴心率增快患者的药物治疗 :首选 兼有减慢心率和降低交感神经兴奋性作用的抗高血 压药物β受体阻滞剂。
(4)高血压伴心率增快的另一类常用降压药 物为非二氢吡啶类钙通道阻滞剂(CCB):该类药物阻断心肌细胞L型钙通道,具有负性肌力、负性传导和负性频率作用,减慢心 率但不抑制交感活性。
(5)If通道阻滞剂伊伐布雷定 :可减慢心率, 对血压基本无影响。对于不能耐受β受体阻滞剂和 非二氢吡啶类CCB的高血压伴心力衰竭或冠心病患 者,可以考虑应用伊伐布雷定。
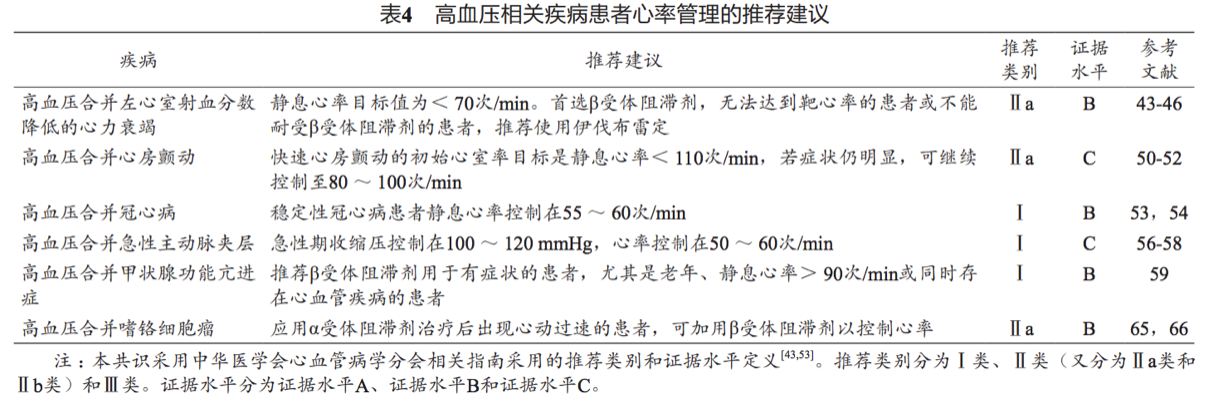
6. 高血压合并特殊疾病的心率管理
(1)积极降压达标能够预 防或推迟心力衰竭的发生及发展,血压应控制在< 130/80 mmHg。
(2)高血压心脏病合并慢 性心房颤动应遵循相应心房颤动指南治疗。
(3)建议将稳定性冠心病患 者的静息心率控制在55 ~ 60次/min。
(4)积极控制血压 和降低心室收缩力,在防止夹层假腔扩张和撕裂的 前提下,尽可能保证组织器官灌注。
(5)心动过速、心 悸见于大多数甲状腺功能亢进症(甲亢)患者,心 率通常为100 ~ 120次/min,严重者可达120 ~ 140 次/min,发生甲亢危象时心率更快。
(6)糖尿病患者常伴有心率增 快,心率增快伴随着增高的全因死亡率和心血管事 件发生率。
(7)嗜铬细胞瘤和副 神经节瘤确诊后应及早行手术治疗,首选α受体阻 滞剂做术前准备,控制高血压。
(8)肥胖与高血压关系密切。 研究显示在超重和肥胖患者中,肌肉交感神经活性 明显增强,并与体质指数、腰臀比和诊室血压均呈 显著正相关。
(9)慢性肾脏病(chronic kidney disease,CKD)患者常常存在交感神经激活, 且交感活性随着肾功能降低而进行性增高,伴随着 心血管、代谢和肾脏病变的加速进展。
(10)高血压合并出血性或缺 血性脑卒中的急性期,可出现交感神经与副交感神 经功能失衡,即交感神经兴奋性相对增高,由此导 致心率改变,临床表现为快速心律失常为主、或快慢交替的心率变化,此时心率干预切点或目标为维 持循环功能稳定。
7. 国外指南和专家共识的观点及建议
(1)欧洲高血压学会2006版《高血压伴心率增 快患者管理共识》中,已有4项研究显示了高血压 患者心率增快伴随着心血管事件和死亡率增高,静 息心率增快能独立预测心血管疾病死亡率。欧洲 高血压学会2016更新版的《高血压伴心率增快患者 管理共识》中,已有12项研究评价了高血压患者心 率增快与心血管事件和死亡率的关系,大多数研究 将静息心率> 80 ~ 85次/min定义为心率增快。这 些研究令人信服地证实了心率增快是心血管疾病的 重要危险因素。尽管还没有随机试验证实药物干预的获益,但在临床实践中对有症状的心率增快患者 可考虑使用减慢心率的药物,首选β1受体阻滞剂。
(2)欧洲心脏病学会/欧洲高血压学会2018版 高血压管理指南 :该指南将静息心率增快(> 80 次/min)列为增加高血压患者心血管事件的独立危 险因素之一,并要求在每次测量血压时同步记录心 率。
(3)印度2019版心率与高血压的专家共识中提 出9点建议,其中几点可供参考 :①尽管高血压患 者的靶心率尚不清楚,但建议使用β受体阻滞剂将 静息心率降至< 70次/min,合并心力衰竭和冠心 病的患者或可降得更低一些 ;②有症状的心率增快 患者(> 80 ~ 85次/min)可使用心脏选择性β1受 体阻滞剂。选择既能减慢心率,又能同时降低外 周动脉血压和中心动脉压的β受体阻滞剂,心率降 低≥ 10次/min就有可能获益。
(4)国际高血压学会2020版高血压实践指南 : 将心率> 80次/min列为高血压患者的危险因素之 一。
8. 临床建议
(1)高血压患者首先强调控制血压达标,兼顾 心率管理。
(2)所有高血压患者在血压测量的同时应测量 诊室静息心率,测量前至少休息5 min,心脏听诊 和脉搏触诊计数心率时的测量时间不应短于30 s, 心房颤动患者的心脏听诊时间应持续至少1 min。
(3)在诊室静息心率> 80次/min时,建议患 者进行家庭静息心率测量,以除外白大衣效应。
(4)我国高血压患者的心率干预切点定义为静 息心率> 80次/min。对高血压合并冠心病、心力衰竭或主动脉夹层患者,应按照相应指南将心率控 制至靶心率。
(5)对于高血压伴静息心率增快的患者,应首 先排查引起心率增快的基础疾病及其他因素,如存 在,宜首先针对原发疾病和诱发因素进行治疗。
(6)高血压伴心率增快的患者应进行有效生活 方式干预。
(7)对高血压伴静息心率增快者,尤其是合并 冠心病、心力衰竭、主动脉夹层及快速心房颤动 (伴心室率增快)的患者,可选择兼有降压和控制 心率作用的药物,如β受体阻滞剂,不能耐受β受 体阻滞剂者可用非二氢吡啶类CCB(HFrEF患者禁用)。应注意药物的不良反应和禁忌证。
(8)优先推荐心脏高选择性长效β1受体阻滞剂 (如比索洛尔、美托洛尔缓释片),对肥胖、血糖增 高和血脂异常患者推荐使用β和α1受体阻滞剂(如 阿罗洛尔、卡维地洛)。
原始出处
中国循证指南共识.中国高血压患者心率管理多学科专家共识 (2021年版).《中国医学前沿杂志(电子版)》2021 年第 13 卷第 4 期.DOI :10.12037/YXQY.2021.04-07
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#专家共识#
38
确实是给了我们临床一个参考,非常好,学习了
65
虽然早就在这么干预,但没证据,这下有了共识
78
#心率管理#
41
学习
62
#多学科#
45
#高血压患者#
28
学习
60