Thyroid:安罗替尼治疗甲状腺髓样癌II期临床研究结果在国际权威杂志发表
2018-08-28 肿瘤资讯编辑部 肿瘤资讯
盐酸安罗替尼作为由我国自主研发的新型口服多靶点酪氨酸激酶抑制剂,在肺癌、软组织肉瘤等领域取得了新进展。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

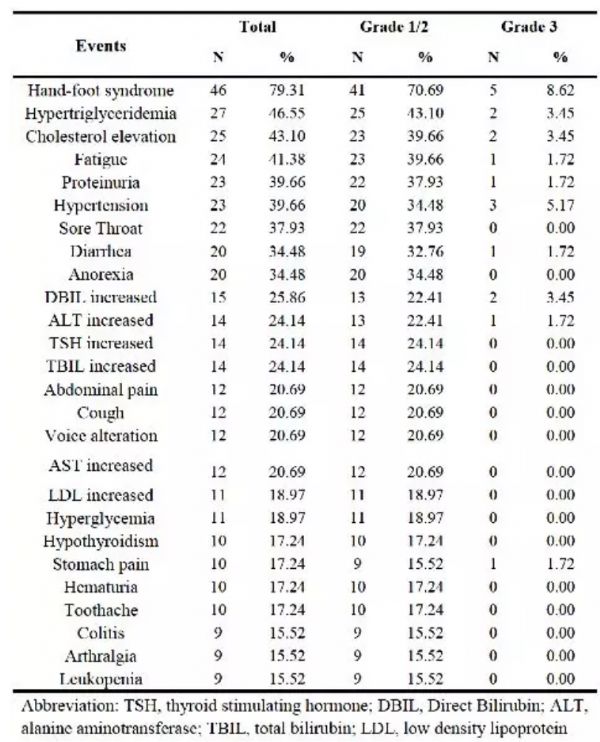







何时用药,后期如何管理
55
#II期临床研究#
35
#髓样癌#
45
#研究结果#
37
#I期临床#
31
很好的学习资料,值得借鉴,学习了,获益匪浅,感谢分享!谢谢
82
#II期临床#
32
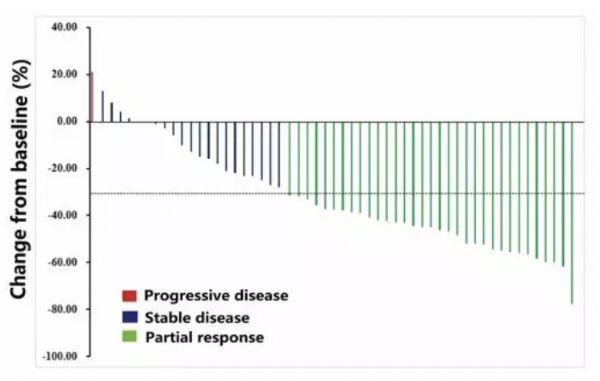
数据还是挺好看
78
嗯嗯,学习学习。
67
谢谢分享,学习了
82