Lancet oncol:结肠癌患者手术治疗后的接受不同医生主导的护理的生活质量
2021-07-05 MedSci原创 MedSci原创
结肠癌患者手术治疗后的第一年内,全科医生主导的护理或可替代外科医生指导的护理
结肠癌与身体和社会心理发病风险增加有关,即使在治疗后也是如此。全科医生 (GP) 护理可能有助于降低这种发病率。本研究旨在对比结直肠癌患者治疗后接受GP主导的生存护理或接受外科医生主导的护理的生活质量(QOL)。此外,并评估了eHealth app(Oncokompas)对QOL的影响。
研究人员在荷兰的八家医院进行了一项务实的2×2析因、开放标签、随机、对照试验,纳入了接受根治性手术治疗的I-III期结肠癌或直肠乙状结肠癌患者,按1:1:1:1随机分成四组,接受由外科医生主导的护理、使用Oncokompas的外科医生主导的护理、GP主导的护理或使用Oncokompas的GP主导的护理。主要终点是5年时的QOL。
2015年3月26日-2018年11月21日期间,共招募了353位患者。50位患者提前撤出研究(27位患者决定的,23位由GP退出的)。在剩余的303位受试患者中,79位被分至外科医生主导的护理组,83位被分至Oncokompas-外科医生主导的护理组,79位被分至GP主导的护理组,68位被分至Oncokompas-GP主导的护理组。
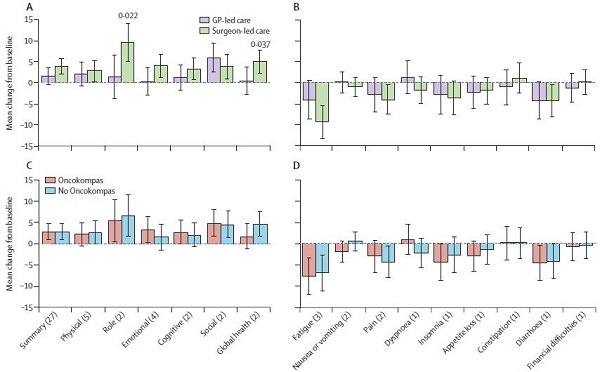
各分组的QOL变化
中位随访了12.2个月(IQR 12.0-13.0)。基线时,所有组的QOL均很高。12个月时,外科医生主导的护理组和GP主导的护理组之间的QOL变化无临床意义的差异;Oncokompas组和非Oncokompas组之间也无明显差异。
在QOL方面,在结肠癌治疗后的第一年内,GP主导的生存护理或可替代外科医生主导的护理。
原始出处:
Julien A M Vos, et al. Effect of general practitioner-led versus surgeon-led colon cancer survivorship care, with or without eHealth support, on quality of life (I CARE): an interim analysis of 1-year results of a randomised, controlled trial. The Lancet Oncology. July 02, 2021. https://doi.org/10.1016/S1470-2045(21)00273-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
39
#Lancet#
31
#手术治疗#
45
厉害了。。
0
学习了#肿瘤#
75
顶刊就是不一样,质量很高,内容精彩!学到很多
53
谢谢梅斯分享这么多精彩信息
53