J Clin Periodontol:根部覆盖手术治疗牙本质过敏的效果如何?
2022-08-26 MedSci原创 MedSci原创
牙本质过敏(DH)被定义为由暴露的牙本质引起的短暂或短暂的剧烈疼痛,通常是对机械、热、化学或渗透性刺激的反应,并且不能归因于任何其他形式的牙齿缺陷或病变。
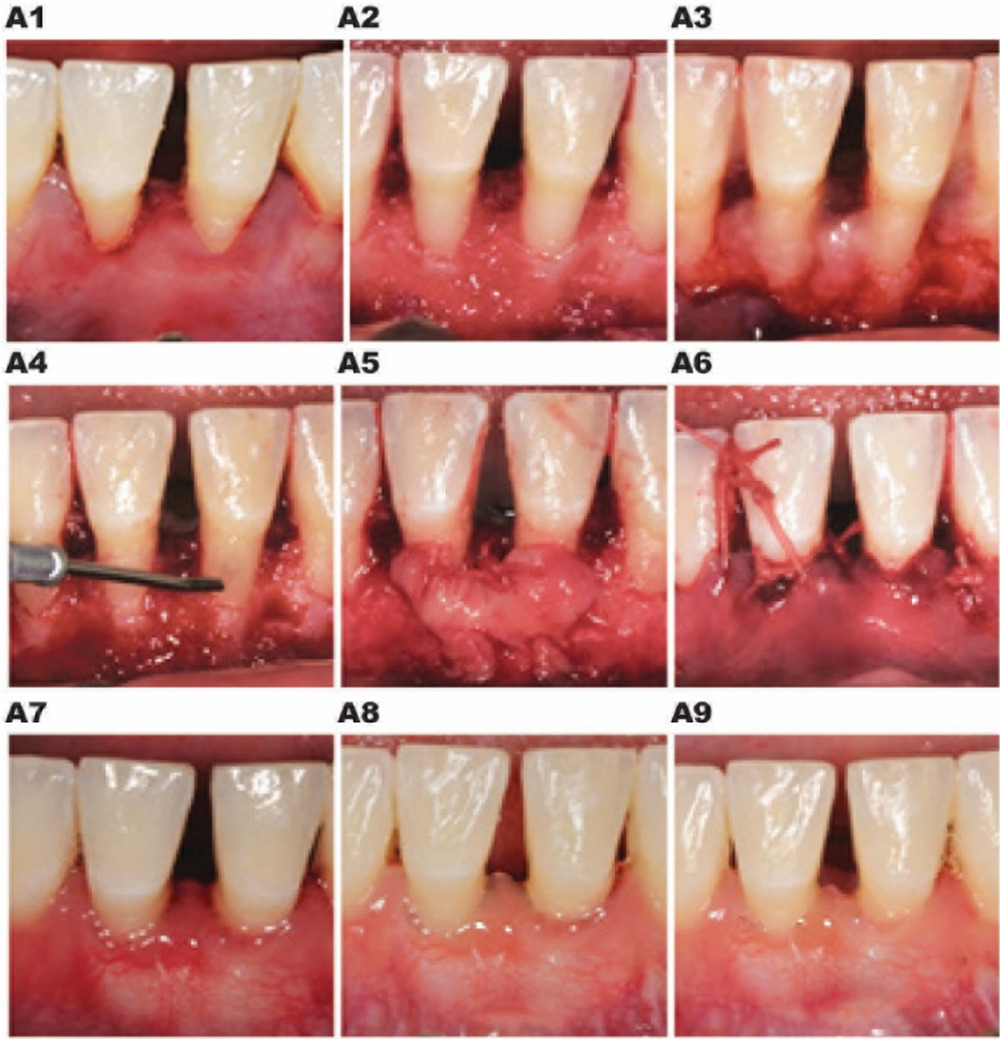
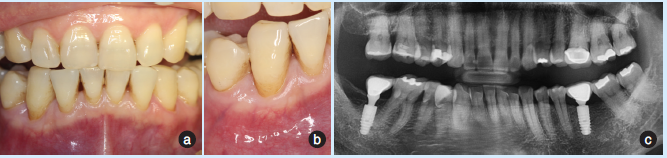
牙本质过敏(DH)被定义为由暴露的牙本质引起的短暂或短暂的剧烈疼痛,通常是对机械、热、化学或渗透性刺激的反应,并且不能归因于任何其他形式的牙齿缺陷或病变。有几种方法被用于治疗DH,包括如脱敏剂和激光治疗。另一个治疗方案是通过覆盖裸露的根面来管理DH。近日,发表于J Clin Periodontol的一项荟萃分析评估了手术根部覆盖(RC)对与牙龈退缩相关的牙本质过敏(DH)的影响。
两位独立评审员对MEDLINE(PubMed)、EMBASE、Cochrane图书馆、Web Of Science、Dentistry & Oral Sciences Source、ScienceDirect和ClinicalTrials.gov数据库进行系统的电子文献检索,以确定2000年1月至2022年3月符合条件的临床研究。纳入的随机对照试验(RCTs)比较了两种外科RC技术或一种外科RC技术联合或未联合辅助治疗。对RCTs提供的数据进行了Meta分析。
结果,研究共纳入了13项RCT,共有701名患者(1086例牙龈退缩)。手术治疗后,DH的抑制率为70.8%(95%置信区间[CI][64.4-76.6];I2=39.2%[3.5-61.8],Q-检验=0.02)。牙龈退缩的减少和RC的百分比都与DH抑制有明显的统计学关系(估计值=0.66[0.10-1.23],p=0.022,R2=14.45%;和估计值=0.04[0.01-0.08],p=0.012,R2=29.54%)。统计学上,冠向复位瓣(CAF)+结缔组织移植的结果比CAF+异体胶原基质的DH抑制更有效(分别为73.3%[65.6-79.8]和61.4%[51.7-70.3];p = 0.048)。

综上所述,该研究结果表明,牙龈退缩手术的成功可显著减少牙本质过敏,改善患者的生活质量。然而,临床医生应该意识到,在RC手术后,大约有三分之一的病例可能持续存在DH,如果牙周参数能够得到改善,应该考虑其他治疗方案,或者考虑二次手术管理。
原始出处:
Angéline Antezack, et al., Effectiveness of surgical root coverage on dentin hypersensitivity: A systematic review and meta-analysis. J Clin Periodontol. 2022 Aug;49(8):840-851. doi: 10.1111/jcpe.13664.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
62
#牙本质过敏#
48
#手术治疗#
46
#牙本质#
48