Radiology:耐受不了结肠镜?双能CT结肠造影为你解忧!
2021-07-19 shaosai MedSci原创
结直肠癌(CRC)是世界上较为常见的恶性肿瘤之一,发病率在中国和美国均居恶性肿瘤的第3位,并且在我国呈逐年上升的趋势。
结直肠癌(CRC)是世界上较为常见的恶性肿瘤之一,发病率在中国和美国均居恶性肿瘤的第3位,并且在我国呈逐年上升的趋势。多数CRC是由腺瘤性息肉经5~15年恶变引起,因此在结直肠疾病的早期进行有效检查尤为重要。结肠镜(CS)能够发现肠内病变,同时能对其定性诊断、活检或治疗;传统CT结肠造影应用于结肠息肉筛查的性能和价值也早已有报道。两者在检查前均需要进行物理肠道准备,充分的肠道准备是保证高质量检查的关键因素。对于有认知障碍和不能耐受的病人,较为复杂的准备过程是造成操作失败率较高的主要原因。
粪便标记法CT结肠造影通过受检者口服对比剂的方法来增加CT结肠造影检查时肠道内部残留物质的对比度,再利用计算机影像后处理将结直肠正常的解剖结构和疾病的变化特点显示出来,因此能够在有效筛查结直肠病变的同时,提高病人对检查的接受程度。然而,粪便标记法的患者间差异较大,并可导致粪便标记不充分,从而降低CT结肠造影检查的可信度。为了克服粪便标记不佳的问题,有研究提出双能CT可以改善对比剂的显示,以增强与息肉之间的对比以有利于进一步的鉴别诊断。低千电子伏(范围,40-60 keV)双能CT虚拟单能重建增强了碘剂的对比度。然而据我们所知,关于双能CT与常规CT在CT结肠造影中息肉检测方面的相关研究仍十分缺乏。
近日,发表在Radiology杂志的一项研究探讨了在体外不同粪便标记水平下双能CT与常规CT相比能否改善结肠息肉的检出率,为双能CT在CT结肠造影中的进一步应用铺平了道路,为临床提供了一个更准确、病人耐受度更高的检测结直肠息肉的影像学手段。
本研究于2017年12月到2019年8月期间,构建了直径30厘米的结肠体模,其中包含60个不同形状(球形,椭圆形,扁平状)和大小(5-9毫米,11-15毫米)的息肉, 并连续填充标记有四种不同碘浓度(每毫升1.26、2.45、4.88和21.00毫克碘)的模拟粪便,然后进行双能CT扫描。 两名阅读者独立评价了常规120 kVp CT和40 keV单能双能CT图像,并记录了息肉的存在和置信度(三点标度)。使用广义估计方程比较传统CT和双能CT之间的敏感性 ,并使用Wilcoxon秩和检验来比较阅读者的信心。
双能CT对息肉的整体检测敏感性高于常规CT (58.8%;95%置信区间[CI]: 49.7%, 67.3%;960个息肉中发现了564个 vs 42.1%;95% CI: 32.1%, 52.8%;在960个息肉中发现了404个,P < .001)。与常规CT图像相比,双能量CT在所有标记水平上的阅读者置信度都有所提高(P < .001)。组间一致性很显著(κ = 0.74;95%CI:0.70,0.77)。
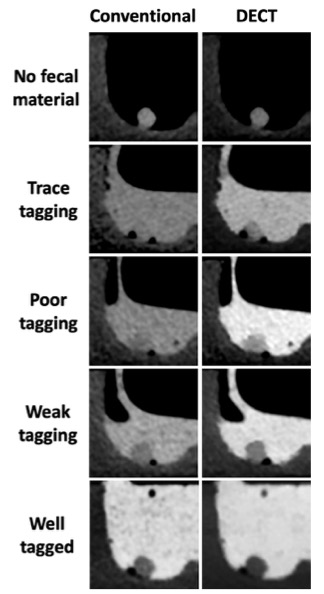
图1 体模CT扫描示例。常规(左)和双能(右)CT扫描的椭圆形息肉(直径8毫米)。每一栏首先显示没有人工粪便物质的息肉,然后在粪便替代物中逐渐增加粪便标记程度(从上到下)。
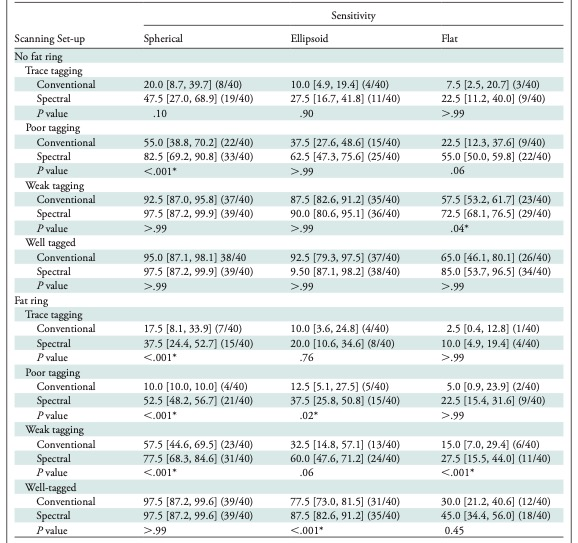
表1 不同息肉形状的息肉检出率的亚组分析。
本研究表明,与传统的120-kVp图像相比,对粪便进行了次优标记的低千电子伏双能量CT结肠造影显著提高了息肉的检测率以及阅读者置信度,对于身体机能处于下降状态及病情危重的患者来说,双能量CT结肠造影无疑为他们提供了一种更加可行的CRC检查手段,同时也为进一步的多中心相关研究开辟了道路。
原文出处:
Markus M Obmann,Chansik An,Amanda Schaefer,et al.Improved Sensitivity and Reader Confidence in CT Colonography Using Dual-Layer Spectral CT: A Phantom Study.DOI:10.1148/radiol.2020200032
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#双能CT#
44
#肠镜#
52
#造影#
32
认真学习
61