喜大普奔!拜耳治疗子宫内膜异位症新药唯散宁®获批上市
2019-05-14 生物谷 生物谷
5月13日,拜耳公司宣布,子宫内膜异位症治疗新药唯散宁®在华获批上市。唯散宁® 是含有2毫克的地诺孕素片剂,是一有效的、普遍耐受良好的子宫内膜异位症的治疗选择,它有效减轻疼痛、缩小病灶、降低术后复发率,可以长期安全使用,提高患者的生活质量,是专门为治疗子宫内膜异位症而研发的药物。子宫内膜异位症是子宫内膜生长在宫腔以外的部位。这种异位的组织也随月经周期而出血脱落。子宫内膜异位的常见部位是卵巢、子宫肌
5月13日,拜耳公司宣布,子宫内膜异位症治疗新药唯散宁®在华获批上市。唯散宁® 是含有2毫克的地诺孕素片剂,是一有效的、普遍耐受良好的子宫内膜异位症的治疗选择,它有效减轻疼痛、缩小病灶、降低术后复发率,可以长期安全使用,提高患者的生活质量,是专门为治疗子宫内膜异位症而研发的药物。
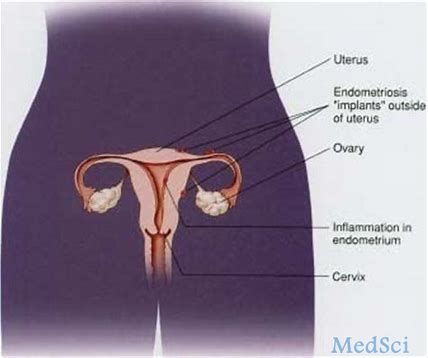
子宫内膜异位症是子宫内膜生长在宫腔以外的部位。这种异位的组织也随月经周期而出血脱落。子宫内膜异位的常见部位是卵巢、子宫肌层和子宫周边组织1。大约有5%到10%育龄女性受此状况影响2,3。子宫内膜异位症可导致渐进性痛经,慢性盆腔痛及性交痛等不同种类的疼痛,有时甚至是重度疼痛;还可能影响生育力4。
育龄女性是子宫内膜异位症的主要易感人群,尽管手术有较好的治疗效果,但子宫内膜异位症的复发率高,术后的药物治疗也很重要5。特别是对于受到疼痛困扰的患者,也主要是通过药物进行缓解。中国医药教育协会妇科专业委员会主任委员,中国医师协会內异症分会副主任委员,北京大学第一医院妇产科副主任周应芳教授表示:“子宫内膜异位症的长期管理目标是减轻和消除疼痛、促进和保护生育能力、降低和减少复发、警惕和早期发现恶变,提高患者的生活质量。”

图:中国医药教育协会妇科专业委员会主任委员,中国医师协会內异症分会副主任委员,北京大学第一医院妇产科副主任周应芳教授
促性腺激素释放激素激动剂(GnRH-a)是目前常用的子宫内膜异位症治疗药物,其疗效确切,常用于短期缓解与子宫内膜异位症相关的症状,考虑到长期使用的安全性问题,如骨密度降低以及潮热等副反应,限制了其长期使用6,7。
周应芳教授表示:“唯散宁®是治疗子宫内膜异位症的重要选择,因为已经证明它可以缓解子宫内膜异位症引起的慢性盆腔疼痛,包括月经疼痛和性交痛,且长期使用副作用小,不会增加潮热盗汗等副反应,不会引起骨密度降低。这是多年来唯一能够长期使用帮助这些患者的新疗法。唯散宁®已被证明对于内异症患者止痛的效果与起效时间与GnRH-a类药物无差异,且疼痛缓解是随着时间推移而持续的(在持续15个月的临床研究中显示),包括痛经、经前期盆腔痛、弥漫性骨盆疼痛和痛觉异常。”
关于唯散宁®
唯散宁®(2mg地诺孕素片)用于治疗子宫内膜异位症。是全球首个专为治疗子宫内膜异位症而研发的孕激素,2009年,唯散宁®(地诺孕素片)获得首次上市许可,当前,唯散宁®已在90多个国家获得上市许可(状态:2014年6月)。累计使用量每年超过15,000,000女性患者。
从一项在252 例子宫内膜异位症患者进行的采用GnRH-a 作为阳性对照的研究中获得的结果证实唯散宁®在疼痛管理的疗效上与GnRH-a相当8,9。一项包括198例子宫内膜异位症患者为期3个月全球研究证实,地诺孕素缓解疼痛显著优于安慰剂10。
在剂量范围研究中,子宫内膜异位症患者接受了24周的地诺孕素片每日治疗,在腹腔镜下,可明显看到地诺孕素片对患者道格拉斯陷凹中子宫内膜异位症病灶的效应11。
一项回顾性队列研究12,比较子宫内膜异位囊肿切除术后(n=568)使用地诺孕素片(n=151)和不使用药物(n=417)人群5年复发率和副作用,超声发现与切除前MRI观察到的大小相等或更大的病灶视为复发。结果显示,术后使用地诺孕素5年累积复发率4%,期待治疗组则高达69%。
地诺孕素中度抑制H-P-O轴,维持体内雌激素处于治疗窗内(即体内雌激素的水平维持在不刺激异位内膜生长而又不引起围绝经期症状如潮热、盗汗等和骨质丢失的范围)8,13,14,长期使用5年12,15和高剂量(20mg或30mg/天,24周)研究16结果显示对血脂、糖代谢等参数无临床意义影响。在临床试验中,唯散宁®一般耐受性良好。最常见的副反应是头痛、乳房不适等,但会随着治疗时间延长而逐渐消失8,17。
数据来源:
1,Dunselman GA, et al. Hum Reprod. 2014.03; 29(3): 400-12.
2,Leyland N et al. J Obstet Gynaecol Can 2010; 32(7 suppl 2): s1–s32.
3,WES. Facts-about-endometriosis Pathophysiology of endometriosis-associated.
4,谢幸、孔北华、段涛. 妇产科学.第9版[M]. 人民卫生出版社, 2018. 262-5.
5,NICE guideline, Endometriosis: diagnosis and management. 2017.
6,Petraglia F et al. Arch Gynecol Obstet 2012;285(1): 1167‒73.
7,Hwang H, et al. Obstet Gynecol Sci, 2018; 61(5): 553-64.
8,Strowitzki T, et al. Hum Reprod. 2010; 25: 633-41.
9,Strowitzki T, et al. Int J Gynaecol Obstet. 2012; 117(3): 228–33.
10,Strowitzki T, et al. Eur J Obstet Gynecol Reprod Biol 2010 Aug; 151 (2): 193-8.
11,Köhler G, et al. Int J Gynaecol Obstet. 2010; 108: 21-5.
12,Ota Y, et al. J Endometr Pelvic Pain Disord. 2015;7(2):63–67
13,子宫内膜异位症的诊治指南[J]. 中华妇产科杂志, 2015(3):161-9.
14,Klipping C et al. J Clin Pharmacol. 2012; 52: 1704-13.
15,Thomas R . Archives of Gynecology and Obstetrics. 2018.
16,Schindler A E, et al. Archives of Gynecology. 2010; 282(5): 507-14.
17,Lang J, et al. J Womens Health (Larchmt). 2018; 27(2): 148-55.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











哟
24
#子宫内膜异位#
38
#获批上市#
38
#内膜#
28
#拜耳#
42