European Radiology:如何鉴别机械性血栓切除术后颅内造影剂外渗与脑内出血?
2022-05-02 shaosai MedSci原创
放射组学是一种从医学图像中提取关键参数的强大工具,是现代医学中指导诊断和治疗的有力工具。
 机械血栓切除术对大血管闭塞具有较高的再通率,可显著改善患者的功能,并可为不符合静脉溶栓条件的患者提供了再通的机会。然而,机械血栓切除术后出现症状性脑内出血的比例在0-7.7%之间。因此,在机械血栓切除术后,早期识别脑实质内出血(IPH)为控制出血良提供了可能,并为术后患者的管理提供重要价值。
机械血栓切除术对大血管闭塞具有较高的再通率,可显著改善患者的功能,并可为不符合静脉溶栓条件的患者提供了再通的机会。然而,机械血栓切除术后出现症状性脑内出血的比例在0-7.7%之间。因此,在机械血栓切除术后,早期识别脑实质内出血(IPH)为控制出血良提供了可能,并为术后患者的管理提供重要价值。
在机械血栓切除术后,常进行平扫计算机断层扫描(CT)以确定治疗的效果,并可评估脑内出血的存在。然而,在CT上很难区分脑内出血和造影剂外渗。在造影剂从血液循环中清除之前,其在成像上仍然可见,这个时间段一般在24小时内。因此,24小时后CT上持续出现的高密度可被认为是出血。然而,机械血栓切除术后0-24小时内出现高密度的患者属于诊断的灰色地带。
放射组学是一种从医学图像中提取关键参数的强大工具,是现代医学中指导诊断和治疗的有力工具。目前,放射组学在脑内出血中的应用是一个不断发展的领域,利用放射组学对血肿异质性进行定量分析是一种可行的方法。由于造影剂和血液内容物具有不同的粘性,放射组学可用于确定机械血栓切除术后CT上高密度的组成评估。
近日,发表在European Radiology杂志的一项研究评估了使用放射组学从碘化造影剂外渗中区分IPH(单纯出血和出血与碘化造影剂混合)的可能性,为该类患者的早期诊断及治疗提供了参考。
本项回顾性研究纳入了2017年12月-2020年6月期间在4家机构接受机械血栓切除术的被诊断为急性缺血性卒中的患者。研究人群被分为训练队列和验证队列。机械血栓切除术后拍摄的平扫CT图像被用来提取放射学特征。使用最大相关性最小冗余(mRMR)算法来消除混杂变量。之后,使用最小绝对收缩和选择算子(LASSO)逻辑回归来生成放射学特征。通过曲线下面积(AUC)、准确性、特异性、敏感性、阳性预测值(PPV)和阴性预测值(NPV)来评估放射学特征的诊断性能。
共使用了101名患者的166个脑内高密度区。这些高密度区域以7:3的比例被随机分配到训练组和验证组。训练队列中放射学特征的AUC为0.848(95%置信区间(CI)为0.780-0.917),验证队列中为0.826(95%CI为0.705-0.948)。在验证队列中,放射组学特征的准确性为77.6%,敏感性为76.7%,特异性为78.9%,PPV为85.2%,而NPV为68.2%。
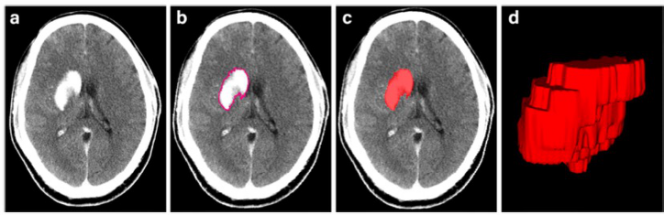
图 使用ITK-SNAP软件划定高信号区。 a 平扫CT上左侧基底节区的高密度区。b 在横断面上沿高密度区轮廓进行人工分割。c 横断面上高密度区的ROI显示为红色区域。d 整个高密度区的三维ROI
本研究表明,基于平扫CT的放射组学特征可以有效区分IPH和机械血栓切除术后早期的碘化造影剂外渗,这为患者的术后管理意义重大。
原文出处:
Xiaojun Chen,Yuanzhe Li,Yongjin Zhou,et al.CT-based radiomics for differentiating intracranial contrast extravasation from intraparenchymal haemorrhage after mechanical thrombectomy.DOI:10.1007/s00330-022-08541-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
33
#切除术#
44
#脑内出血#
38
#血栓切除#
38
#血栓切除术#
45
#机械性血栓切除术#
42
#造影#
39