Acta Neuropathologica: 儿童幕上室管膜瘤:不仅仅是RELA或YAP
2021-01-29 MedSci原创 MedSci原创
室管膜瘤是在儿童和年轻人中第二常见的恶性颅内肿瘤。在儿童时期,室管膜瘤发生在中枢神经系统(CNS)内的所有部分,最常见的位置是后颅窝,其次是幕上和脊柱部位。
室管膜瘤是在儿童和年轻人中第二常见的恶性颅内肿瘤。在儿童时期,室管膜瘤发生在中枢神经系统(CNS)内的所有部分,最常见的位置是后颅窝,其次是幕上和脊柱部位。基于组织学上的相似性,不同部位的室管膜瘤在过去被认为是一个整体。室管膜瘤中的各种潜在遗传变化被纳入2016年WHO脑肿瘤分类。
据研究报道,幕上室管膜瘤与RELA融合是一个独特的实体。目前已经鉴定出七种不同的RELA融合变体,这些肿瘤约占儿童幕上室管膜瘤的70%。除室管膜瘤伴RELA融合外,YAP1-MAMLD1融合的肿瘤被认为是第二个出现在儿童幕上室的实体。与伴有不良预后的RELA融合肿瘤相比,YAP1-MAMLD1融合的室管膜瘤预后良好。
在这项研究中,我们报告了18例儿童非RELA/非YAP幕上室管膜瘤,通过其组织学、免疫表型、遗传学和表观基因组学对其进行了系统的特征描述。全面的分子分析包括高分辨率拷贝数分析、甲基化分析、通过Nanostring技术分析融合转录物和RNA测序。
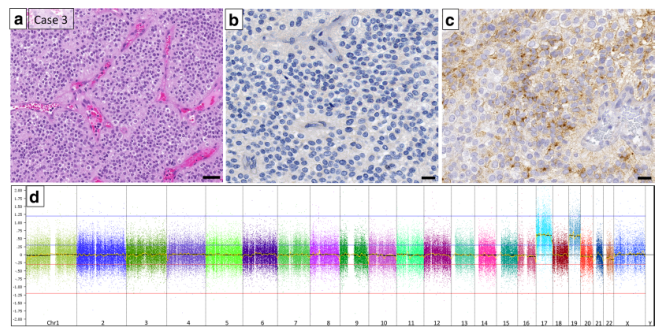
根据组织学和免疫组化特征,本研究确定了两种主要类型--RELA样室管膜瘤(9例)和伸展细胞室管膜瘤(6例)。在组织学上属于WHO III级并类似于RELA融合的室管膜瘤的RELA样组中,肿瘤缺乏p65-RelA的核表达作为NF-κB通路病理激活的替代标记。三个肿瘤显示出与MAML2或NCOA1的C11orf95选择性融合。一个基于甲基化的脑肿瘤分类器将两个RELA样肿瘤归为甲基化类"EP,RELA-融合"; 其他的没有显示出显著的相似性。在伸展细胞室管膜瘤组中,5/6的肿瘤被定为WHOⅡ级,同时未检测到基因融合,甲基化分析未显示与已建立的甲基化类别有任何关联。
本研究数据表明,除了目前发现的室管膜瘤外,至少还存在两种幕上室管膜瘤类型(RELA型和伸展细胞型)。本研究建议对幕上室管膜瘤进行综合组织病理学和遗传学诊断,以便准确识别这些肿瘤并进一步定性。
Zschernack, V., Jünger, S.T., Mynarek, M. et al. Supratentorial ependymoma in childhood: more than just RELA or YAP. Acta Neuropathol (2021). https://doi.org/10.1007/s00401-020-02260-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#YAP#
48
#CTA#
42
#pathologic#
45
#Pathol#
34
#管膜瘤#
45
#室管膜瘤#
40
#室管膜瘤#
40