BMJ Support Palliat Care:电针治疗可有效改善老年女性的压力性尿失禁
2022-06-02 sunshine MedSci原创
EA可能是治疗老年和非老年妇女SUI或压力为主的MUI的有效和安全的替代疗法。年龄可能不会影响电针的治疗效果。
尿失禁,即非自愿性的尿液流失,是女性常见的抱怨常见于女性。压力性尿失禁(SUI)或压力为主的混合性尿失禁(MUI)的特点是在体力消耗、打喷嚏或咳嗽时尿液不自主地从尿道口漏出。近日,发表于BMJ Support Palliat Care的一项随机对照研究比较了电针(EA)对老年和非老年妇女SUI或MUI的疗效。
本研究是对两项随机对照试验的二次分析,纳入了252名SUI妇女和132名以压力为主的MUI妇女,均接受了相同的EA方案治疗。老年妇女被定义为年龄大于60岁者。主要研究结果是,从基线到第6周,平均72小时尿失禁发作频率(IEF)下降≥50%的患者比例。总体而言,在SUI和MUI试验中共招募了1004名妇女。在EA组中,基线时以急迫性为主或平衡型MUI的患者被排除在本次研究之外,因此最终的样本量为384人。
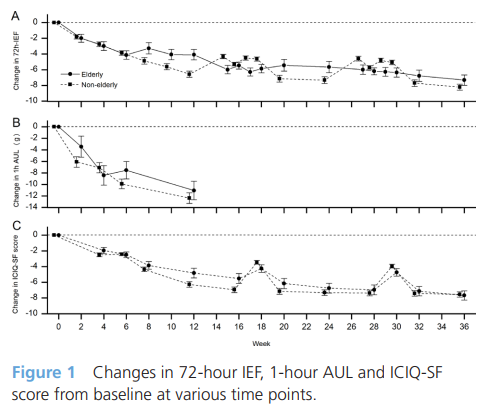
结果,在384名接受EA治疗的SUI或压力为主的MUI患者中,371人完成了研究。分析结果显示,经过6周的治疗,72小时平均IEF比基线下降≥50%的女性比例,老年组为57.3%(51/89),非老年组为60.70%(173/285);组间差异不大(3.11%,95%CI-9.83%至16.05%;P=0.637)。在第4、16和28周观察到类似的结果。两组患者的72小时IEF、漏尿量(通过1小时尿垫测试评估)和国际失禁症调查问卷-短表得分都比基线有所下降,组间差异不明显。研究期间没有观察到明显的EA相关不良事件。
综上所述,该研究结果表明,EA可能是治疗老年和非老年妇女SUI或压力为主的MUI的有效和安全的替代疗法。年龄可能不会影响电针的治疗效果。
原始出处:
Biyun Sun, et al., Electroacupuncture for stress-related urinary incontinence in elderly women: data analysis from two randomised controlled studies. BMJ Support Palliat Care. 2022 May;12(e1):e164-e170. doi: 10.1136/bmjspcare-2019-002034.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#BMJ#
60
#电针#
32
#support#
38
#尿失禁#
52
#ALL#
43