王长利教授畅谈非小细胞肺癌靶向治疗领域热点问题
2018-01-26 肿瘤资讯编辑部 肿瘤资讯
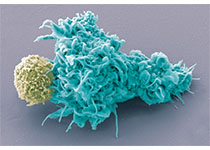
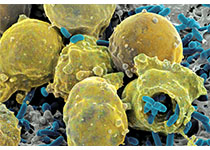
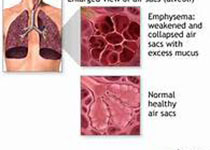
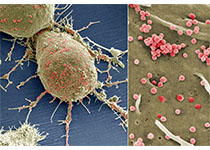
随着精准医学时代的到来,以驱动基因为靶点的分子靶向治疗和抑制免疫检查点的免疫治疗成为了肺癌治疗的新方向。在过去的几年中,分子靶向治疗和免疫治疗领域都取得了突破性进展,但临床实践中仍然会遇到许多令人困惑的问题:早期非小细胞肺癌辅助靶向治疗的现状? 靶向辅助治疗在临床中该如何应用?【肿瘤资讯】就以上热点问题采访了王长利教授。
王长利教授天津医科大学肿瘤医院副院长 天津医科大学肿瘤医院肺部肿瘤科主任 中国抗癌协会肺癌专业委员会主任委员 天津市抗癌协会肺癌专业委员会主任委员 天津市肺癌诊治中心主任
肿瘤资讯:ADJUVANT、EVAN研究开启非小细胞肺癌辅助靶向治疗新篇章,将靶向治疗推向早期肺癌,王长利教授请您分析一下早期非小细胞肺癌辅助靶向治疗的现状?
王长利教授:最近这半年多,术后辅助靶向治疗一直是大家热议的话题,因为过去我们一直在晚期肺癌中研究EGFR通路,取得了很好的成绩,但是在术后辅助靶向治疗领域一直是很困惑,十几年来国内国外的III期临床研究和回顾性研究都没有很好的数据。2017年我们在这方面获得了可喜的突破,ADJUVANT研究和EVAN研究都获得了成功。这两个研究都得到了同样的结论,术后辅助靶向治疗是安全、可行的,能给患者带来获益,这对我们今后临床实践有很大的指导意义。虽然要在近期真正改变指南可能还需要一些数据,但至少这两个研究取得了很好的结果,我想这就是大家如此关注这一领域的原因。
对于临床实践中到底应该如何应用,我认为在指南改变之前医生仍需要慎重考虑。临床医生需要跟病人深入沟通。我个人建议可以将其作为一个选择,对于IIIa期有EGFR基因突变,还是可以推荐其做术后辅助靶向治疗。
肿瘤资讯:王长利教授,ADJUVANT、EVAN研究为国内肺癌患者打开全新的生存局面,辅助靶向治疗将成为趋势,早期肺癌的诊治格局迎来重大变革。在术后辅助靶向治疗上,您认为辅助治疗多长时间最佳?
王长利教授:这两个研究历经了六七年的时间得出结论,非常不容易。与以往晚期肺癌的II期、III期临床研究不同,这两个试验时间跨度非常大,好在目前看来这两个试验还是很超前的,设计没有落后,对现在的临床实践也有指导意义。大家都很关注用药时间,当时我们选择时间的时候比较困惑,主要考虑了以下两个因素:第一,N2的病人的中位生存时间只有十几个月,所以我们选择的用药时间应该覆盖这个时间;第二,在晚期肺癌中,靶向药物本身耐药时间大概是十几个月,所以我们选择了两年。目前还没有充分的证据和数据能够给出这一问题的答案,从我的经验和对临床试验的观察来看,我认为2年是最恰当的,1年时间略短一些,因为IIIa期、N2的病人他的进展时间大约十几个月,我们需要覆盖这个时间。实际上大家知道,2年之后大部分病人会出现耐药,因此2年以上的给药时间太长了。但是因为我们没有做足够的检验,所以目前2年是不是最合理的给药时间,仍不明确。
肿瘤资讯:面对晚期的非小细胞肺癌患者,在分子检测上您会做一些改变吗?
王长利教授:我认为现在临床上基因检测有一点落后,临床同行们在这方面应保持正确认识。随着精准治疗的开展,基因检测是必需的,没有基因检测,精准治疗将成为空谈。二代检测更具优势,因为外显子突变、基因融合和扩增的检测可同时完成,这可以为病人的治疗决策的选择上提供更充分的证据。若仅行单基因检测,得到阴性结果后还要换一个单基因进行检测,非常费时、繁琐。所以我认为二代检测应该是精准医学治疗中更实用的方法,更应该优先开展。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#非小细胞#
31
#热点问题#
22
#肺癌靶向治疗#
36
谢谢分享.
68
继续关注.
60
继续学习.
54