Crit Care:入住ICU时的血浆谷氨酰胺水平是危重病患者死亡的独立危险因素
2021-07-08 MedSci原创 MedSci原创
ICU入院时高谷氨酰胺血症是一个独立的死亡率预测因子,但并非总与急性肝病相关。
据报道,重症监护病房(ICU)入院时血浆谷氨酰胺浓度超出正常范围与患者死亡率增加相关。尽管有研究经常报道低谷氨酰胺血症,但迄今为止报道高谷氨酰胺血症患者的数量十分有限。

近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,在这项前瞻性观察性研究中,研究人员分析了高谷氨酰胺血症与死亡率结局之间的关联。

该研究受试者的排除标准为18岁以下、再次入院、无知情同意或入院时“不复苏”医嘱。在受试者入院后一小时内留取血样,通过高压液相色谱分析了谷氨酰胺浓度。受试者入院时进行常规风险评分(简化急性生理学评分和顺序器官衰竭评估),研究人员记录所有纳入患者的死亡率结局。
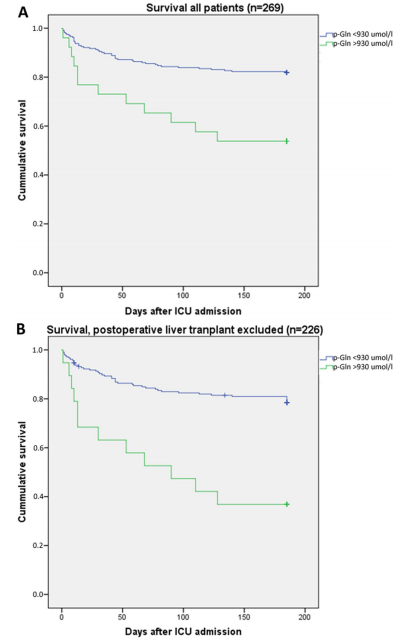
生存曲线
269名患者被纳入研究,26名患者入院时伴有高谷氨酰胺血症(≥930µmol/L)。该亚组6个月的死亡率为46%,而血浆中谷氨酰胺浓度<930µmol/L(P=0.002)的患者死亡率为18%。回归分析表明,高谷氨酰胺血症是一个独立的死亡率预测因子,它为常规入院风险评分和年龄增加了预测价值。
由此可见,ICU入院时高谷氨酰胺血症是一个独立的死亡率预测因子,但并非总与急性肝病相关。血浆谷氨酰胺浓度超出正常范围的机制,以及在ICU住院期间重复测量血浆谷氨酰胺的预后价值,仍有待深入研究。
原始出处:
Marie Smedberg.et al.Plasma glutamine status at intensive care unit admission: an independent risk factor for mortality in critical illness.Critical Care.2021.https://ccforum.biomedcentral.com/articles/10.1186/s13054-021-03640-3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#危重病#
46
#独立危险因素#
44
#患者死亡#
32
学习
57
学习
79
学习
65
好喜欢
67