EHJ:三血管疾病患者,使用全新技术PCI术后明显改善生存率!
2021-10-11 MedSci原创 MedSci原创
与最初SYNTAX I试验中使用PCI治疗的预定义患者相比,在新发三血管疾病患者中使用SYNTAX II PCI策略可获得更好和持久的临床效果。
针对三支血管(3VD)和/或左主干冠状动脉疾病(LMCAD)患者的冠状动脉血运重建的最佳策略一直都存在激烈的争论。针对3VD的随机对照试验和大型观察性研究一致表明,冠状动脉旁路移植(CABG)的死亡率明显低于经皮冠状动脉介入(PCI)。
SYNTAXES试验为期10年随访,该试验是第一个评估新发3VD和/或LMCAD患者在使用药物洗脱支架(DES)进行PCI后与CABG的≥10年生存率的随机试验。总的来说,该研究显示,CABG组和PCI组的全因死亡率相似;然而,CABG确实明显改善了3VD患者的生存率。
近期,SYNTAX II研究评估了PCI的进展对新发三血管疾病患者预后的影响,这些进展被整合到一个单一的血管再造策略中。该研究利用SYNTAX评分II进行决策,使用冠状动脉生理学、薄层可降解聚合物药物洗脱支架、血管内超声、加强对慢性全闭塞的治疗以及优化药物治疗。结果发表在近期《欧洲心脏病杂志》EHJ上。
SYNTAX II是一项多中心、单臂、开放标签的研究,研究对象是需要进行血管重建的患者,根据SYNTAX评分II预测,这些患者在临床上适合接受CABG或PCI治疗。主要终点是主要不良心脑血管事件(MACCE),其中包括任何血管再造。比较者是一个匹配的PCI队列试验和一个匹配的CABG队列,均来自SYNTAX I试验。
总的来说,5年后,SYNTAX II的MACCE率明显低于SYNTAX I PCI队列(21.5% vs. 36.4%)。这反映了较低的血管重建率(13.8% vs. 23.8%)和心肌梗死(MI)(2.7% vs. 10.4%),包括程序性MI(0.2% vs. 3.8%)和自发性MI(2.3% vs. 6.9%)。
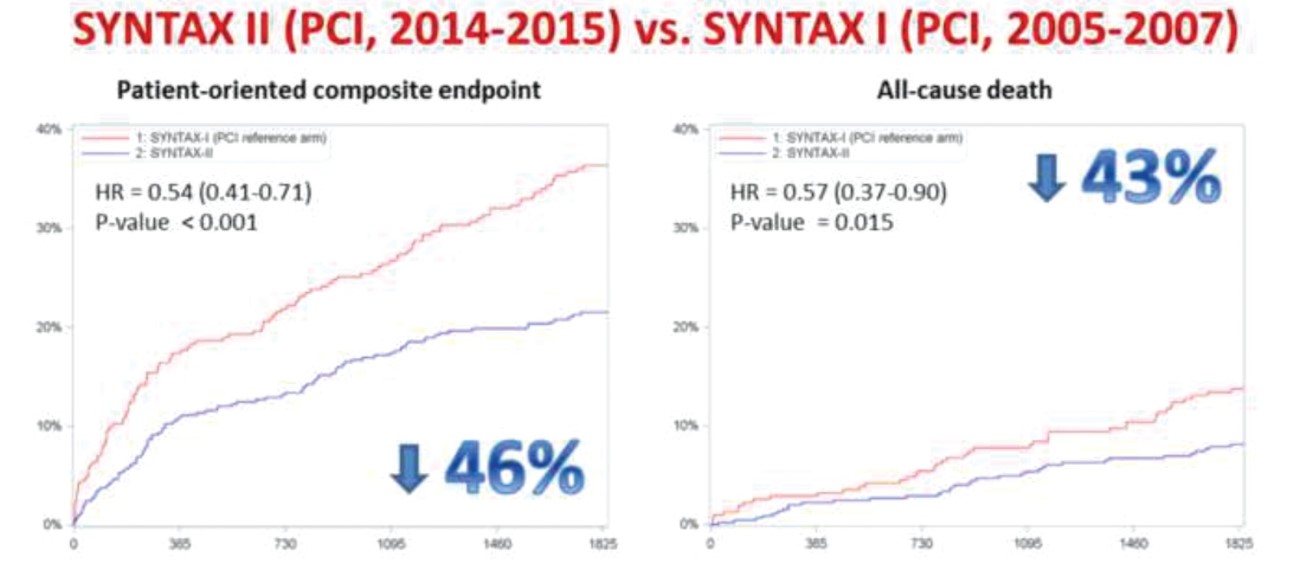
SYNTAX I与SYNTAX II试验的MACCE发生率比较
同时,SYNTAX II的全因死亡率较低(8.1% vs. 13.8%),反映出心脏死亡率较低(2.8% vs. 8.4%)。SYNTAX II的患者和SYNTAX I CABG队列中预定的患者在5年内的主要不良心脑血管事件的结果相似(21.5% vs. 24.6%)。
综上,与最初SYNTAX I试验中使用PCI治疗的预定义患者相比,在新发三血管疾病患者中使用SYNTAX II PCI策略可获得更好和持久的临床效果。
参考文献:
Five-year outcomes after state-of-the-art percutaneous coronary revascularization in patients with de novo three-vessel disease: final results of the SYNTAX II study, European Heart Journal, 2021;, ehab703, https://doi.org/10.1093/eurheartj/ehab703
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















赞
35
#PCI术#
49
#疾病患者#
40
#新技术#
50
#生存率#
47
#PCI术后#
52
#血管疾病#
34