纳入优先审评!恒瑞医药创新药吡咯替尼新适应症——新辅助治疗
2021-09-26 恒瑞医药 恒瑞医药
近日,恒瑞医药创新药马来酸吡咯替尼片联合曲妥珠单抗加多西他赛用于表皮生长因子受体 2(HER2)阳性早期或局部晚期乳腺癌患者的新辅助治疗的注册申请获国家药品监督管理局受理,被国家药品监督管理局药品审评
近日,恒瑞医药创新药马来酸吡咯替尼片联合曲妥珠单抗加多西他赛用于表皮生长因子受体 2(HER2)阳性早期或局部晚期乳腺癌患者的新辅助治疗的注册申请获国家药品监督管理局受理,被国家药品监督管理局药品审评中心纳入拟优先审评品种公示名单。此次被纳入优先审评程序,将有助于吡咯替尼该适应症药品注册申请早日获批,为乳腺癌患者提供一种新型的新辅助治疗方案。
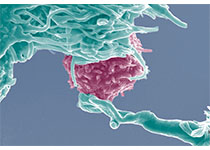
根据2020年世界卫生组织国际癌症研究机构(IARC)发布的数据,乳腺癌已成为全球第一大恶性肿瘤,是女性最常见的恶性肿瘤之一。统计数据表明,2020年全世界新确诊的女性乳腺癌患病人数约有226万例。在我国,2020年中国癌症数据显示,乳腺癌发病率占全身各种恶性肿瘤发病率的9.1%(41.64万);乳腺癌患者死亡病例约11.72万例。目前国内患者乳腺癌发病率增长迅速,已经位列女性肿瘤发病谱首位,并且近50%患者治疗后会出现复发和转移。按照乳腺癌的分子分型,乳腺癌分为luminal型(激素受体阳性型)、HER2(人表皮生长因子受体2)过表达型以及三阴性乳腺癌。
新辅助治疗是针对早期或局部晚期乳腺癌的术前治疗,长期以来被用于缩小肿瘤以使不可手术转变为可手术,并能提高保乳率,还可以降低腋窝分期。新辅助治疗的病理完全缓解(pCR)的情况与早期乳腺癌的无病生存期(DFS)和总生存期(OS)相关。早期乳腺癌患者的病理反应和远期生存之间的相关性在三阴性乳腺癌患者中最强,HER2阳性患者次之,激素受体阳性患者的相关性最小。在新辅助治疗的临床实践中,抗HER2治疗联合化疗能够显著提高患者的pCR率并改善患者的转归,确立了目前HER2阳性乳腺癌新辅助治疗的标准模式。同时大量进行中或已完成的临床试验也在努力挖掘其他靶向治疗联合化疗在HER2阳性乳腺癌新辅助治疗的疗效潜力。
吡咯替尼是恒瑞医药自主研发的创新药,是一种小分子、不可逆、泛ErbB受体酪氨酸激酶抑制剂,是中国首个原研EGFR/HER2靶向药物,也是中国首个凭借Ⅱ期临床研究获CFDA有条件批准上市的治疗实体瘤的创新药。吡咯替尼于2018年08月获得有条件批准上市,联合卡培他滨用于治疗HER2阳性、既往未接受或接受过曲妥珠单抗治疗的复发或转移性乳腺癌患者,使用前患者应接受过蒽环类或紫杉类化疗,并于2020年07月获得该适应症的完全批准。
本次注册申请是基于吡咯替尼联合曲妥珠单抗加多西他赛新辅助治疗HER2阳性的早期或局部晚期乳腺癌的一项随机、双盲、安慰剂对照、多中心的III期临床研究,结果显示,吡咯替尼联合曲妥珠单抗加多西他赛新辅助治疗HER2阳性早期或局部晚期乳腺癌患者,可显著提高患者的总体病理完全缓解率。
目前,恒瑞医药正在开展吡咯替尼在HER2阳性乳腺癌中的多项临床研究,涉及乳腺癌在疾病发展不同阶段的治疗用药。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#医药创新#
29
#新辅助#
21
#优先审评#
34
#创新#
24
#适应症#
32
#医药#
21
#新适应症#
36
期待在肺癌上能有更好表现
51