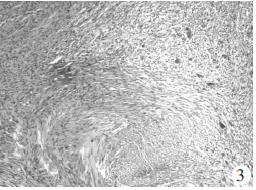
颅内神经鞘瘤伴海绵状血管瘤一例
2019-02-13 黄燕涛 冷媛媛 实用医学影像杂志
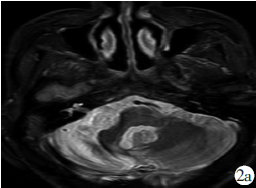
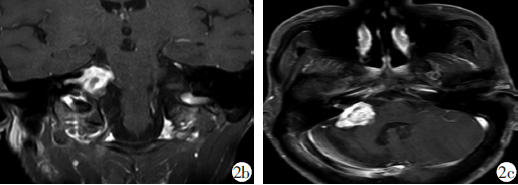
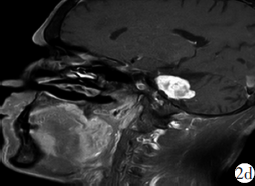
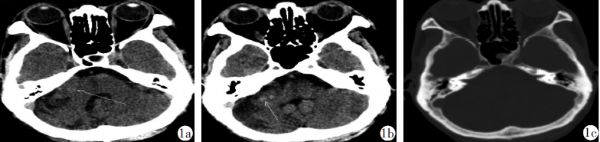
患者男,57岁,因“右侧阵发性耳鸣”来院就诊;颅脑CT平扫示右侧桥小脑角区见不规则软组织密度影,CT值约37Hu,大小约2.8 cm×1.2 cm,密度不均匀,其内见斑结状稍高密度影(CT值约50Hu),邻近脑组织稍受压,右侧内听道较左侧略增宽(图1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#神经鞘瘤#
44
#血管瘤#
33
#海绵状血管瘤#
38
#海绵状#
36