尽管进行了广泛的基础和临床研究,动脉硬化性心血管疾病(ASCVD)仍然是全世界最常见的死亡原因。人们普遍认为,低密度脂蛋白胆固醇(LDL-C)是动脉粥样硬化的最重要风险因素,在ASCVD的发展中起着因果作用。尽管有效、安全的降胆固醇药物已广泛使用,但大多数人的循环LDL-C水平仍超过最佳水平。
后来Bumcrot等人认识到干扰特定RNA的治疗潜力。因此,一类新的药物,小分子干扰核糖核酸(siRNA)已经在开发中。其中,PCSK9抑制剂可以降低循环中的LDL-C,改善ASCVD患者或高风险患者的临床预后。然而,这种降低LDL-C的方法有两个问题,特别是对于无症状者的ASCVD的初级预防。(i) 抗体的半衰期相对较短,需要多年来每2或4周进行一次皮下注射,也许是终生注射,这导致了对长期坚持的担忧,以及(ii) 当用于没有ASCVD证据的无症状者的一级预防时,需要相对大量的抗体,导致相对较高的成本。

后来,有学者发现,LDL-C的致动脉粥样硬化作用似乎取决于循环LDL-C的水平和这种水平的持续时间。半个多世纪以来,人们已经知道家族性高胆固醇血症患者在早期就会发生ASCVD。另一方面,编码PCSK9的基因功能缺失等位基因仅导致LDL-C在一生中适度降低,但与ASCVD的发展明显减少有关。
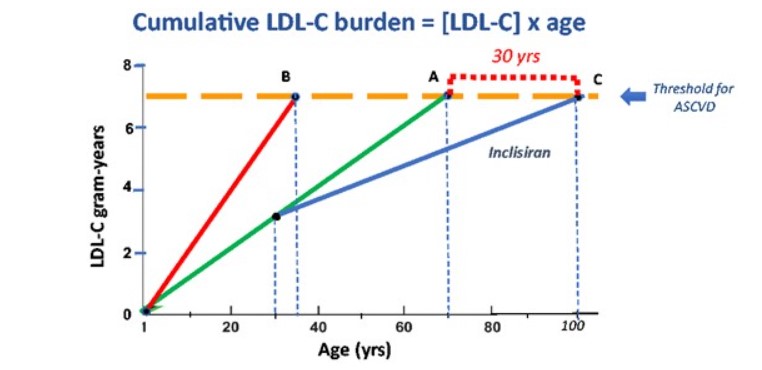
为此,动脉粥样硬化负担可以用 "胆固醇·年 "或 "LDL-C·年 "表示,类似于吸烟包年。Horton等人提出,当以毫克-年或克-年表示的LDL-C-年的累积负担达到一个阈值时,ASCVD的临床证据就会显现。
作者建议,从30岁开始给予A所代表这类个体每年一次长效降脂药物治疗,其LDL-C水平有望从100 mg/dL降至60 mg/dL(即C线),动脉粥样硬化负荷的进展速率也将因此下降。30年后,当受试者达到100岁时,将达到7克-年的ASCVD阈值。
此外,达到ASCVD阈值的延迟也取决于受试者开始使用降脂药的年龄——越早越好。另外,没有考虑这种新药长期间歇性治疗可能产生的不良反应,也没有考虑在降低LDL-C的几十年里可能出现的LDL-C浓度变化。
综上,在每年注射流感(和可能的冠状病毒)疫苗的基础上,增加基于siRNA的降脂药物将有望进一步控制LDL-C,从而大大延缓ASCVD的发生。
参考文献:
How to live to 100 before developing clinical coronary artery disease: a suggestion, European Heart Journal, Volume 43, Issue 4, 21 January 2022, Pages 249–250, https://doi.org/10.1093/eurheartj/ehab532
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#皮下注射#
40
#siRNA#
60
#重磅#
29