Eur J Cancer:EGFR突变型肺癌的组织学转化概率及临床病程
2022-03-18 xiaozeng MedSci原创
约3%的对EGFR-TKI获得性耐药的EGFR突变的非小细胞肺癌患者会发生组织学转换
肺癌是全球癌症相关死亡的首要原因。非小细胞肺癌(NSCLC)约占所有肺癌的80%;大部分病例首次确诊时已发生转移,丧失手术机会。据报道,约50%的亚洲晚期NSCLC患者携带EGFR基因酪氨酸激酶结构域的体细胞激活突变。
本研究是一项多中心、回顾性的队列研究,纳入了2012年至2019年期间接受EGFR酪氨酸激酶抑制剂(TKI)治疗的EGFR突变的晚期肺癌患者,旨在明确有组织学转换的EGFR突变的肺癌的发生率和临床病程。主要评估指标是组织转换的发生率。次要指标是有组织转换的患者的治疗效果。
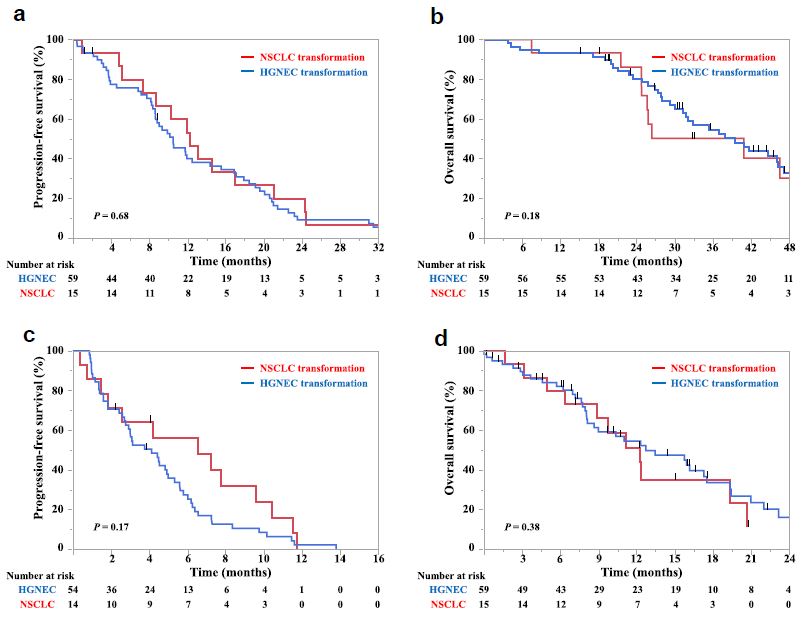
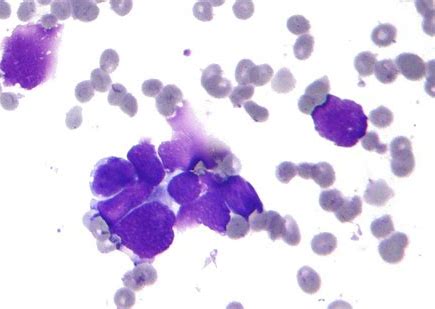
不同情况患者的无进展生存期或总生存期
总体上,共招募了6356位患者。2624位患者在对EGFR-TKI产生了获得性耐药后活检明确了组织学类型,其中74位存在组织学转换(发生率 2.8%)。对EGFR-TKI产生了获得性耐药后的中位无进展生存期是10.4个月;发生了组织学转换后首次治疗后的中位无进展生存期是4.4个月,组织学转换的方向(转换成高级别神经内分泌癌或另一种非小细胞肺癌)对患者的生存期无明显影响。确认组织学转换后的总生存期是12.2个月。
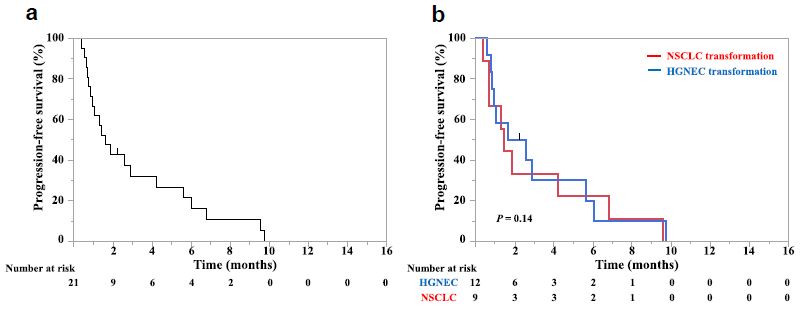
组织学转换后或根据有无组织学转换分组的接受ICI治疗后的无进展生存期
27位患者接受免疫检查点抑制剂治疗,其中确认组织学转换前6例,确认组织学转换后21例。无患者获得1年无进展生存期。证实HT后接受免疫检查点抑制剂治疗后的中位无进展生存期为1.6个月。
综上,约3%的对EGFR-TKI获得性耐药的EGFR突变的非小细胞肺癌患者会发生组织学转换。遗憾的是,免疫检查点抑制剂在这类患者中的治疗效果有限。
原始出处:
Fujimoto Daichi,Akamatsu Hiroaki,Morimoto Takeshi et al. Histologic transformation of epidermal growth factor receptor-mutated lung cancer.[J] .Eur J Cancer, 2022, 166: 41-50.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#组织学#
37
#组织学转化#
31
#突变型#
43
#临床病程#
32
#GFR#
30