Eur J Heart Fail:射血分数降低的心力衰竭患者达格列净与房颤的关系
2021-11-26 MedSci原创 MedSci原创
与安慰剂相比,达格列净降低了伴有AF和不伴有AF患者发生HF恶化、心血管死亡和全因死亡的风险,并改善了患者的症状。
在射血分数降低的心力衰竭(HFrEF)患者中,伴有心房颤动(AF)对某些治疗的反应可能与不伴有AF的患者完全不同。

近日,心血管领域权威杂志European Journal of Heart Failure上发表了一篇研究文章,研究人员在达格列净和预防心力衰竭不良结局试验(DAPA-HF)中调查了达格列净对伴有和不伴有AF的HFrEF患者中的疗效和安全性,此外,研究人员还分析了达格列净对新发AF的影响。
该研究的主要结局是心衰恶化(心衰住院或需要静脉输液治疗的心衰急诊)或心血管死亡的复合结局。在随机分配的4744名患者中,1910名(40.3%)有“任何AF”(房颤病史或心电图检查结果上的AF)。与安慰剂相比,达格列净在伴有和不伴有任何AF的患者中以相似的程度降低了HF恶化或心血管死亡的风险[风险比(HR)分别为0.75,95%置信区间(CI)为0.62-0.92和0.74,95%CI为0.62-0.88;交互作用的p=0.88]。
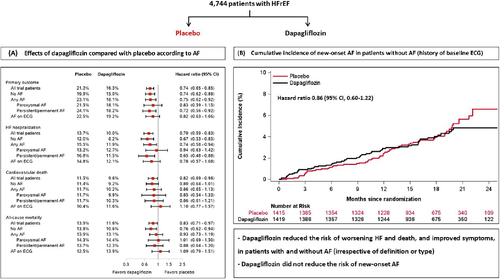
在主要结果的组成部分、全因死亡率和堪萨斯城心肌病问卷总症状评分的改善方面,研究人员观察到了一致的益处。在基线时不伴有AF的患者中,与安慰剂相比,达格列净并未显著降低新发AF的风险(HR为0.86,95%CI为0.60-1.22)。然而,与未发生AF的患者相比,新发AF患者的不良结局风险高出5至6倍。
由此可见,与安慰剂相比,达格列净降低了伴有AF和不伴有AF患者发生HF恶化、心血管死亡和全因死亡的风险,并改善了患者的症状。此外,达格列净并未降低新发AF的风险。
原始出处:
Jawad H. Butt.et al.Dapagliflozin and atrial fibrillation in heart failure with reduced ejection fraction: insights from DAPA-HF.European journal of heart failure.2021.https://onlinelibrary.wiley.com/doi/10.1002/ejhf.2381
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ART#
45
#射血分数降低#
74
#HEART#
40
已学习
68
这研究太详细了
65