THER ADV NEUROL DISO:动脉瘤性蛛网膜下腔出血血管内治疗后预后预测模型
2022-06-25 影像小生 MedSci原创
对于血管内治疗后的aSAH患者,所提出的预后预测模型优于经典评分系统,尤其是当经典评分系统未能对aSAH评分良好的患者做出任何有价值的预测时,而后者占该临床人群的大多数(79%)。
颅内动脉瘤破裂引起的蛛网膜下腔出血是一个世界性的健康负担,其特点是高致死率和永久致残率。大约三分之一的患者在动脉瘤性蛛网膜下腔出血(aSAH)后的最初几周内死于严重的脑损伤,大部分幸存者遭受长期残疾或认知障碍。aSAH后患者的预后预测模型不仅对告知预后预期至关重要,而且对确定有利预后的可改变因素也至关重要。然而,临床严重程度和动脉瘤特征之间复杂的相互作用如何共同决定aSAH后的预后尚不清楚。
THER ADV NEUROL DISO最近刊发了复旦大学华山医院Han Lu等的研究成果,该研究旨在设计一种准确的aSAH患者血管内治疗后的预后预测模型,并阐明临床严重程度与动脉瘤特征之间的相互作用。

该研究使用1029例接受血管内治疗的aSAH患者的临床均质数据来建立预后模型。动脉瘤特征通过变量来衡量,如动脉瘤大小、颈部大小和圆顶颈比,而入院时的临床严重程度通过共病和神经系统状况来衡量。共使用18个临床变量进行预后预测。考虑到在这个临床人群中有利结果和不利结果之间的不平衡,该研究同时使用集成学习和深度强化学习方法进行预测。
该研究发现:
随机森林(RF)模型是预测所有患者预后的最佳方法,对分级良好的aSAH患者也是如此。该模型使用独立的检验数据集进行了准确的预测(AUC = 0.869±0.036,敏感性= 0.709±0.087,特异性= 0.805±0.034),入院时的临床严重程度是预测的主要因素。
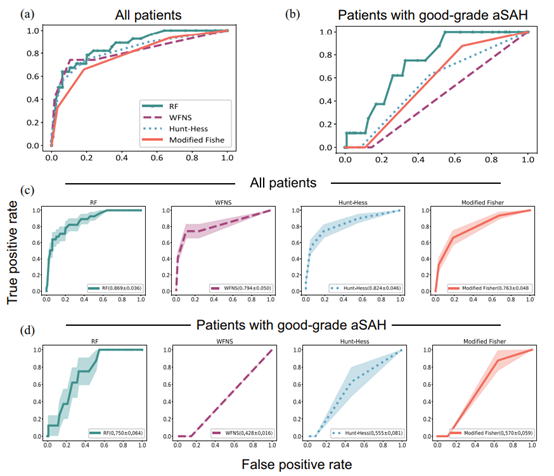
使用测试数据集比较模型性能。使用独立测试数据集比较各模型的受试者工作特征(ROC)曲线。(a)所有患者训练各模型的平均ROC曲线。(b)使用临床严重程度分级良好的患者训练各模型的平均ROC曲线。(c)所有患者训练的每个模型的ROC曲线标准差。(d)使用临床严重程度分级良好的患者训练的各模型ROC曲线的标准差。
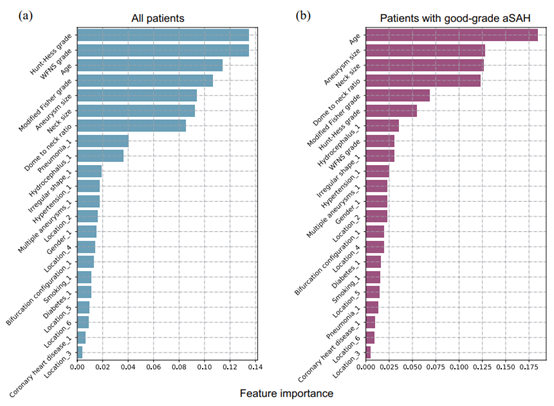
特征对预后预测的贡献排名。(a)对所有aSAH患者训练的RF模型的贡献。(b)使用临床严重程度等级良好的患者训练RF模型的贡献。
对于分级良好的aSAH患者,RF模型表现最佳(AUC = 0.805±0.034,敏感性= 0.620±0.172,特异性= 0.696±0.043),动脉瘤特征是主要因素。经典的评分系统在该患者组失败(AUC < 0.600;敏感性= 0.000,特异性= 1.000)。
该研究利用迄今为止样本量最大的临床均质数据集建立了一种对血管内治疗后的aSAH患者的预后预测模型。与使用独立测试数据集进行的基于经典临床量表的预测相比,该预测模型表现更好,特别是当经典评分系统无法对高分级aSAH患者做出任何有信息的预测时。
原文出处
An accurate prognostic prediction for aneurysmal subarachnoid hemorrhage dedicated to patients after endovascular treatment
https://journals.sagepub.com/doi/full/10.1177/17562864221099473
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Neurol#
42
#蛛网膜#
60
#Dis#
37
#预测模型#
44
#动脉瘤性蛛网膜下腔出血#
43