Science封面重磅:mRNA注射可在体内直接制造CAR-T细胞,一针修复心脏
2022-01-07 医诺维 医诺维
CAR-T细胞疗法,用患者的T细胞并对其进行基因工程改造,以在其表面表达称为CAR的特殊受体,用来识别特定抗原。然后将产生的CAR-T细胞输回患者体内,以发现并攻击表面具有抗原的细胞。
CAR-T细胞疗法,用患者的T细胞并对其进行基因工程改造,以在其表面表达称为CAR的特殊受体,用来识别特定抗原。然后将产生的CAR-T细胞输回患者体内,以发现并攻击表面具有抗原的细胞。人们往往会把CAR-T疗法中的CAR形容为导航,带着T细胞找到目标细胞。
纤维化是许多严重疾病的基础,包括心力衰竭、肝病和肾衰竭。心力衰竭的重要诱因是心肌纤维化,成纤维细胞长期过度产生使心肌变硬,并损害心脏功能。然而,疗法却非常有限。
2022年1月6日,美国宾夕法尼亚大学佩雷尔曼医学院的研究人员在国际顶尖期刊" Science "上发表了一篇题为" CAR T cells produced in vivo to treat cardiac injury "的研究论文,该研究刊登期刊封面。
该研究表明,mRNA注射可在体内直接制造CAR-T细胞,仅通过单次注射mRNA就可攻击特定目标,成功攻击了小鼠的心脏成纤维细胞,恢复心力衰竭小鼠的心脏功能。
CAR-T细胞疗法目前主要用于治疗癌症,但在许多其他疾病中,也有显着的成果。
早在2019年,该研究的研究人员就表明,标准的CAR-T细胞方法可用于攻击过度活跃的心脏成纤维细胞,并可以恢复心力衰竭小鼠的心脏功能。然而,当针对人类的心力衰竭或其他纤维化疾病时,这种疗法却出现了问题。
众所周知,成纤维细胞在人体内具有重要的功能,尤其是在伤口愈合方面。然而,经过基因重编程以攻击成纤维细胞的CAR-T细胞可以在体内存活数月甚至数年,它会一直抑制成纤维细胞数量,降低伤口愈合能力。
在该研究中,研究人员设计了一种新技术,针对于短期、可控、程序简单的CAR-T细胞疗法类型。
具体来说,研究人员设计了一种编码靶向活化成纤维细胞的T细胞受体的mRNA,并将其封装在脂质纳米粒(LNP)中,而这些脂质纳米粒本身也被T细胞上的分子所覆盖。
当注射到小鼠体内,封装的mRNA分子与T细胞结合,并作为产生成纤维细胞靶向受体的模板,有效地重新编程T细胞以攻击活化的成纤维细胞。
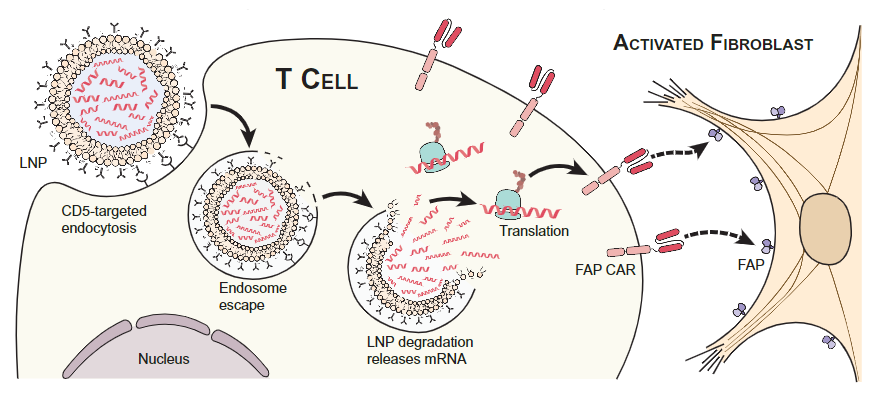
在体内制造CAR-T细胞,攻击成纤维细胞
值得注意的是,这种重新编程是短暂的。mRNA没有整合到T细胞DNA中,在T细胞内仅存活几天,几天后T细胞恢复正常,不再靶向成纤维细胞。
研究人员发现,尽管mRNA只在T细胞中存活短短的几天,但在心力衰竭的小鼠模型中注射这种mRNA,可以成功地重新编程大量T细胞,能使小鼠的心脏纤维化大大减轻,恢复了大部分正常心脏功能。
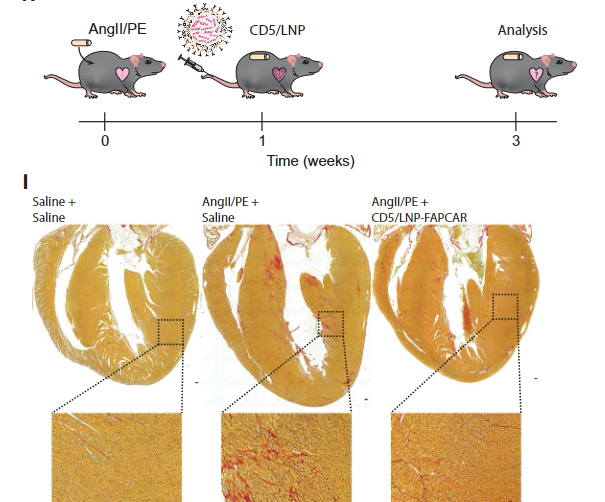
小鼠的心脏纤维化大大减轻
重要的是,在治疗一周后,研究人员发现,小鼠体内没有抗纤维化的T细胞持续存在。
研究人员表示,标准的CAR-T细胞疗法很昂贵,并且很难在普通疾病和贫穷国家使用,而这种在体内制造功能性的CAR-T细胞疗法极大地拓展了mRNA/LNP平台的前景。
目前,研究人员正在继续测试这种基于mRNA的短暂CAR-T细胞技术,希望最终能够应用于临床试验。
原始出处:
JOEL G. RURIK ISTVáN TOMBáCZ AMIR YADEGARI, et al. CAR T cells produced in vivo to treat cardiac injury. SCIENCEVOL. 375, NO. 657606 JAN 2022 : 91-96.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CAR-#
32
#SCIE#
25
#重磅#
36
学习了。
66
能否用于肝硬化
70
值得拥有
0
学习
49
涉及基因及自身系统里修复,希望带来好的**
59
1周后小鼠体内没有抗纤维化的T细胞持续存在,这似乎并不符合CAR-T 特征
36
虽然这篇文章发表在顶刊上,但是大家不要迷信,将来这篇文章被质疑的概率应该极高。至少有如下几点难以解释,作者很有可能隐藏了某些数据: 1 为什么是CD5,而不是CD3?CD5不应该产生如此效应? 2 没有报道对其它器官的副作用 3 心脏中的T细胞数量是极低的,这个CAR-T有用??还能展示如此强的表型! 4 纤维化不严重,动物模型似乎并不可靠。 5 心肌功能几乎完全恢复,很难进行解释,即使是有效,那些已肥大,或纤维化的细胞功能也很难完全恢复
0