Eur Radiol:DSC-PWI,实现了胶质母细胞瘤和转移瘤的术前无创鉴别!
2022-05-10 shaosai MedSci原创
对神经放射学家来说,最具挑战性的鉴别方法之一是胶质母细胞瘤(GB)与单发脑转移瘤,这是成人最常见的两种恶性颅内肿瘤。
 众所周知,脑肿瘤的术前诊断对病人的治疗至关重要。虽然组织病理学仍然是最终的参考标准,但外科手术前主要依赖于以磁共振(MR)为主导的神经影像学进行诊断及评估。对神经放射学家来说,最具挑战性的鉴别方法之一是胶质母细胞瘤(GB)与单发脑转移瘤,这是成人最常见的两种恶性颅内肿瘤。在神经肿瘤科,患者是否有已知的颅外原发肿瘤是一个经常争论的问题,能否在手术前区分这两种肿瘤将大大影响进一步的治疗决策。因此,在临床实践中,使用非侵入性的检测方法实现最高的诊断准确性是一个尚未满足的关键需求。
众所周知,脑肿瘤的术前诊断对病人的治疗至关重要。虽然组织病理学仍然是最终的参考标准,但外科手术前主要依赖于以磁共振(MR)为主导的神经影像学进行诊断及评估。对神经放射学家来说,最具挑战性的鉴别方法之一是胶质母细胞瘤(GB)与单发脑转移瘤,这是成人最常见的两种恶性颅内肿瘤。在神经肿瘤科,患者是否有已知的颅外原发肿瘤是一个经常争论的问题,能否在手术前区分这两种肿瘤将大大影响进一步的治疗决策。因此,在临床实践中,使用非侵入性的检测方法实现最高的诊断准确性是一个尚未满足的关键需求。
然而,这两种类型的肿瘤在表现上具有高度的异质性,而形态学上的MR往往受到限制,无法达到可信赖的诊断。出于这个原因,近年来,在这种情况下,所谓的高级或功能性MR成像技术的使用越来越多,其中DSC-PWI技术就是其中之一。
研究表明,DSC-PWI与肿瘤血管化、微血管和血脑屏障完整性的不同组织学特征相关。GB的特点是异质性的血脑屏障破坏,而在转移瘤中并不存在血脑屏障,而血管生成是最主要的现象。关于瘤周区域,转移瘤会引起纯粹的血管性水肿,而在GB的水肿中可能会发现浸润的肿瘤细胞。
许多学者试图根据DSC-PWI对GB和转移瘤进行术前区分,在不同的研究中使用了许多不同的灌注参数,其结果和阈值具有高度的异质性。评价最多的经典参数是脑血容量(CBV)、信号恢复百分比(PSR)和峰值高度(PH),这些都是从DSC-PWI的时间强度曲线(TICs)中提取得来。研究表明,分析和比较整个TIC而不是这些具体的参数可能会提供更好的信息,通过归一化的TIC(nTIC)可以单独比较训练预测模型。
近日,发表在European Radiology杂志的一项研究提出了一种鉴别胶质母细胞瘤和转移瘤的DSC-PWI nTICs体素级强度直方图分析的新方法,并测试了其临床鉴别的效能,为临床术前进行无创的准确诊断提供了有价值的影像学工具。
本项回顾性研究检索了经组织学确认的胶质母细胞瘤或单发脑转移的患者,并对每位患者进行了包含DSC-PWI序列的MR扫描。在CE-T1WI上对增强的肿瘤和紧邻的肿瘤周围区域进行分割,并将其与DSC-PWI进行核心登记。分段的时间强度曲线被归纳为正常外观的白质。获得每个参与者归一化曲线的平均值和所有体素矩阵。在每种类型的肿瘤之间选择10个最好的鉴别时间点。然后,对这10个时间点中的每一个进行强度直方图分析,为每一个时间点选择最佳鉴别性的体素百分位。使用二元逻辑回归法对增强型肿瘤和肿瘤周围区域进行单独的分类模型训练。
共有428名患者(321名胶质母细胞瘤,107名转移瘤)符合纳入研究(256名男性;平均年龄,60岁;范围,20-86岁)。在训练和测试集中分离胶质母细胞瘤和转移灶的结果令人满意,AUCs为0.71-0.83,独立准确率为65-79%,综合准确率达81-88%。
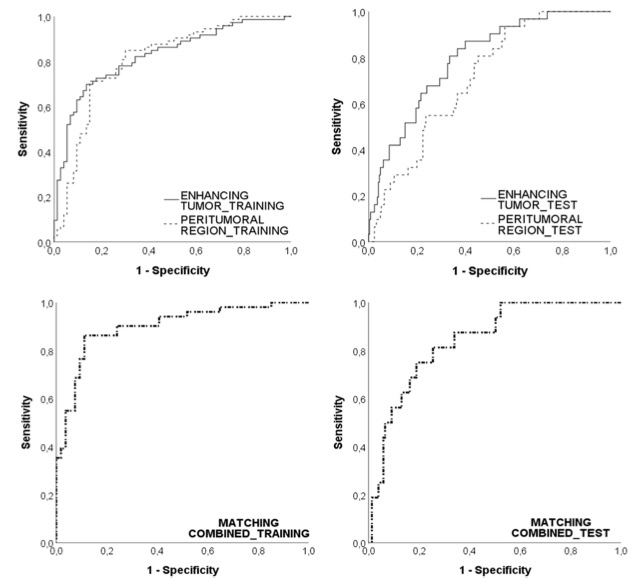
图 训练组(左)和测试组(右)的AUC-ROC曲线,增强的肿瘤(线)、瘤周区(虚线)和匹配组合(下行)。训练组(增强型肿瘤AUC=0.81,瘤周区AUC=0.83,匹配组合AUC=0.90)。测试组(增强肿瘤AUC=0.79,瘤周区域AUC=0.71,匹配组合AUC=0.84)。均有统计学差异(P<0.00015)
本项研究为DSC-PWI分析提供了一个新的视角,超越了对CBV、PSR或PH等孤立参数及其平均值或极端值的解释。本研究的新方法提供了一种对操作者依赖性最小的技术,可用于分析归一化灌注曲线中的每一个时间点以及肿瘤和瘤周区域的每一个体素,实现了在手术前对胶质母细胞瘤和转移灶的准确鉴别。
原文出处:
Albert Pons-Escoda,Alonso Garcia-Ruiz,Pablo Naval-Baudin,et al.Voxel-level analysis of normalized DSC-PWI time-intensity curves: a potential generalizable approach and its proof of concept in discriminating glioblastoma and metastasis.DOI:10.1007/s00330-021-08498-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PWI#
32
#胶质母细胞#
35
#转移瘤#
36
#母细胞瘤#
51
学习了
46
#细胞瘤#
40