双特异性抗体Faricimab治疗AMD的Ⅲ期数据公布,16周仅需给药1次
2020-05-14 MedSci MedSci原创
AMD是老年群体中常见的一种眼部疾病,影响视力的中心区域——黄斑,这是人视觉最敏锐和最关键的部位。AMD分为“湿性(wet)”和“干性&rd
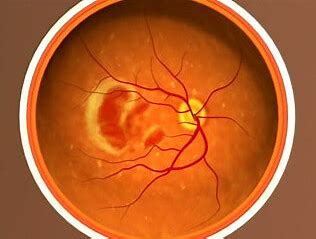
AMD是老年群体中常见的一种眼部疾病,影响视力的中心区域——黄斑,这是人视觉最敏锐和最关键的部位。AMD分为“湿性(wet)”和“干性”2种类型,前者更为严重。wet-AMD也称为nAMD,其特点是黄斑部视网膜后出现异常新生血管并在黄斑下生长和渗漏,造成黄斑损害,同时导致疤痕组织破坏中央视网膜,这一过程可在几个月到几年的时间内导致视力下降,甚至失明。全球范围内约有1700万人患有nAMD,该病是导致65岁以上老年群体严重视力损害和失明的主要原因。
目前有4种抗VEGF新药(贝伐单抗、雷珠单抗、阿柏西普、康柏西普)已在临床得到广泛应用,表现出良好的治疗效果。阿柏西普、雷珠单抗以及康柏西普这几种药物都存在共同的缺点:注射液剂型,需要通过玻璃体内给药,极其不便。nAMD患者每个月或每2-3个月进行玻璃体内注射,患者的依从性较差,治疗负担大。
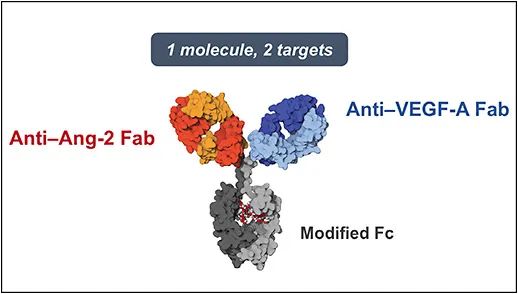
Faricimab是专门为玻璃体内注射而设计的首个双特异性抗体,可同时强效及特异性结合并中和Ang-2(血管生成素-2)和VEGF-A(血管内皮生长因子A)。
近日,罗氏(Roche)公布了双特异性抗体Faricimab(Ang-2/VEGF-A)的最新临床数据,在52周最新临床数据中,每隔12周或每16周注射一次Faricimab的患者在视力和解剖学方面表现出“可比”的改善。例如,对于16周的Faricimab,12周的Faricimab和4周的Lucentis,病变部位分别缩小4.2毫米,5.4毫米和4.5毫米。提示,在治疗AMD第52周时,与4周一次的Lucentis给药组相比,16周一次的faricimab给药组与前者显示出相当的持续视力改善效果。
Faricimab着眼于DME与湿性AMD
Ang-2水平升高,提示视网膜血管损伤、周细胞减少和视网膜微血管炎性反应,这一信号在DR和DME病理机制方面具有重要作用。Faricimab是首个被设计用于眼内治疗的双特异性抗体药物,一个分子针对VEGF-A Fab和Ang-2 Fab两个靶点,其中拮抗Ang-2的作用有助于提高视网膜血管稳定性。
在nAMD中,Ang-2和VEGF协同作用驱动病理性血管通透性和不稳定性、异常的血管生长和液体渗漏,从而导致视力丧失。Ang-2在nAMD炎症的多个方面也起着重要作用。Ang-2信号传导通路与血管不稳定性和微血管炎症有关,而VEGF-A可以促进新生血管生成,因此Faricimab可以增强相关眼科疾病患者的血管稳定性、减少新生血管的形成、减轻炎性渗出等,理论上可起到更好的治疗效果。
faricimab临床试验包括针对DME患者的2期研究BOULEVARD,针对湿性AMD患者的AVENUE,STAIRWAY和两个相同设计的3期TENAYA和LUCERNE研究等。
BOULEVARD研究的主要观察指标是,随访24周后对于初始DME患者与雷珠单抗相比faricimab的有效性。共计229例患者入组,被分为6.0mg faricimab组、1.5 mg faricimab组和0.3 mg 雷珠单抗组,治疗方案是按月治疗。
结果显示24周后3组患者平均最佳矫正视力(BCVA)均能提高2行以上,6.0 mg faricimab组BCVA稍高于雷珠单抗组(3.6个字母,P=0.03,80%CI,1.53~5.61)。该研究还观察的次级终点包括,(1)视力提高超过2行的患者比例:其中以往接受过抗VEGF治疗的患者中,6.0mg faricimab组比雷珠单抗组相结果更佳;(2)CST变化:CST下降方面三组无显著差异,但事后分析中,CST≤325µm的患者比例这一指标,6.0mg faricimab组比雷珠单抗组相结果更佳;(3)DR改善≥2级的患者比例:三组结果无显著性差异。此外研究还观察了药效持续情况和不良事件情况。
将近1,300名患有湿性AMD的患者将被纳入两个相同设计的3期TENAYA和LUCERNE研究中。该研究将评估faricimab与Eylea(aflibercept,Regeneron)相比治疗湿性AMD的安全性,有效性和耐久性。患者将被随机分配,每16周接受一次faricimab治疗,可选择每12周或8周治疗一次,或者每8周一次aflibercept治疗。两项研究的主要终点是第48周从基线开始的最佳矫正视力的变化。预计在2022年或2023年结束。
此前报道:雷珠单抗和阿柏西普的新对手 它将如何改变湿性AMD市场格局?
参考出处:
相关文献:
Simultaneous Inhibition of Angiopoietin-2 and Vascular Endothelial Growth Factor-A with Faricimab in Diabetic Macular Edema: BOULEVARD Phase 2 Randomized Trial.Ophthalmology . 2019 Aug;126(8):1155-1170. doi: 10.1016/j.ophtha.2019.03.023.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#特异性#
0
#mAb#
40
双特异性抗体是热点,但是也不一定都有效!
77
#AMD#
40
#特异性抗体#
46
#faricimab#
45