这项指标正常就能安心了?即使是正常高值,全因死亡风险升高近30%!
2022-01-09 LILYMED MedSci原创
BMC Nephrol. :中国社区老年人群尿白蛋白与肌酐比值及全因死亡率的关系:一项10年随访研究
随着老龄化加速,预测中老年人全因死亡风险的工具,在研究政策和临床实践中变得越来越重要。慢性肾脏病(CKD)定义为存在蛋白尿和/或肾功能下降,是终末期肾病(ESKD)、心血管事件和全因死亡的/重要危险因素。在一般人群中,蛋白尿与全因死亡之间的关系受到广泛关注。蛋白尿在老年人中非常普遍,尤其是糖尿病和高血压患者。然而,它对老年人健康以及社区全因死亡率的总体影响尚未得到详细研究。 尿白蛋白与肌酐的比例是监测尿蛋白排泄的一种新的可靠方法。尿白蛋白与肌酐比值的测量可以可靠地反映24小时内尿蛋白的量。而且它快速,简单,准确,,已成为蛋白尿的临床定性和定量诊断指标,可取代传统的24小时尿蛋白定量。
研究表明,高水平的尿白蛋白排泄与心血管(CV)死亡率的增加有关,特别是在糖尿病和高血压患者以及有心血管疾病史的患者中,但很少有关于预测社区人群全因死亡率的研究。本研究通过从社区人群中选取了一个相对较大的队列,随访了10年,从多个层面研究了尿白蛋白与肌酐比值与全因死亡率的关系。
参与者来自中国北京万寿路社区,招募工作始于2010年。平均年龄为71.48岁,女性比例为60.1%。共有2148人完成了随机尿液样本,以确定尿白蛋白与肌酐比值(UACR)。受试者根据UACR分为三组:第1组(UACR<10 mg / g),第2组(10 mg / g <UACR<30 mg / g),第3组(UACR>30 mg / g)。使用Kaplan-Meier生存分析和Cox回归模型来验证UACR与全因死亡率之间的关系。图1显示了研究人群的招募过程。
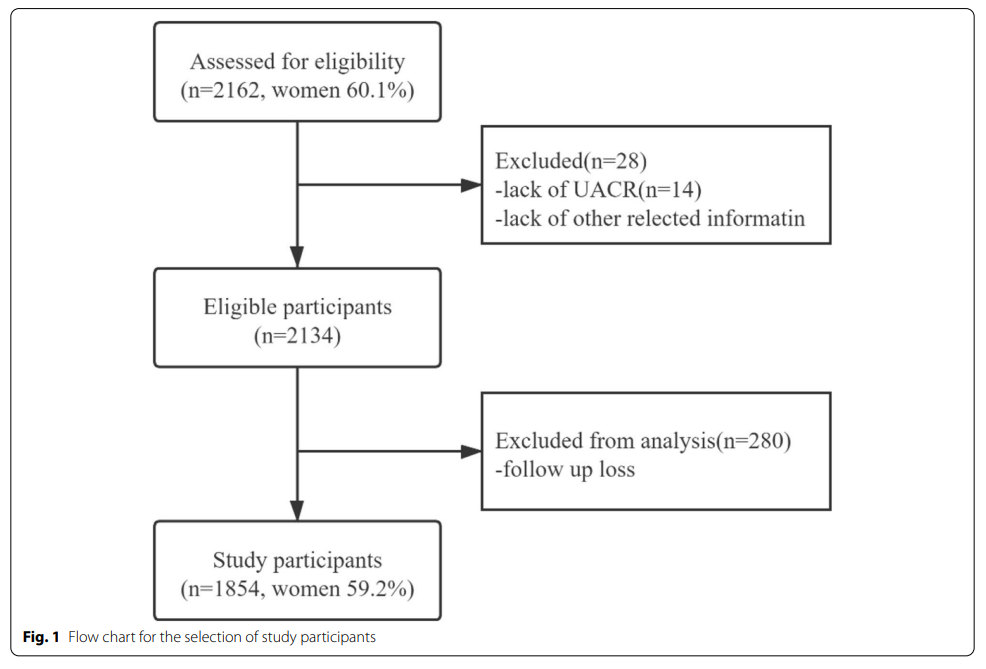
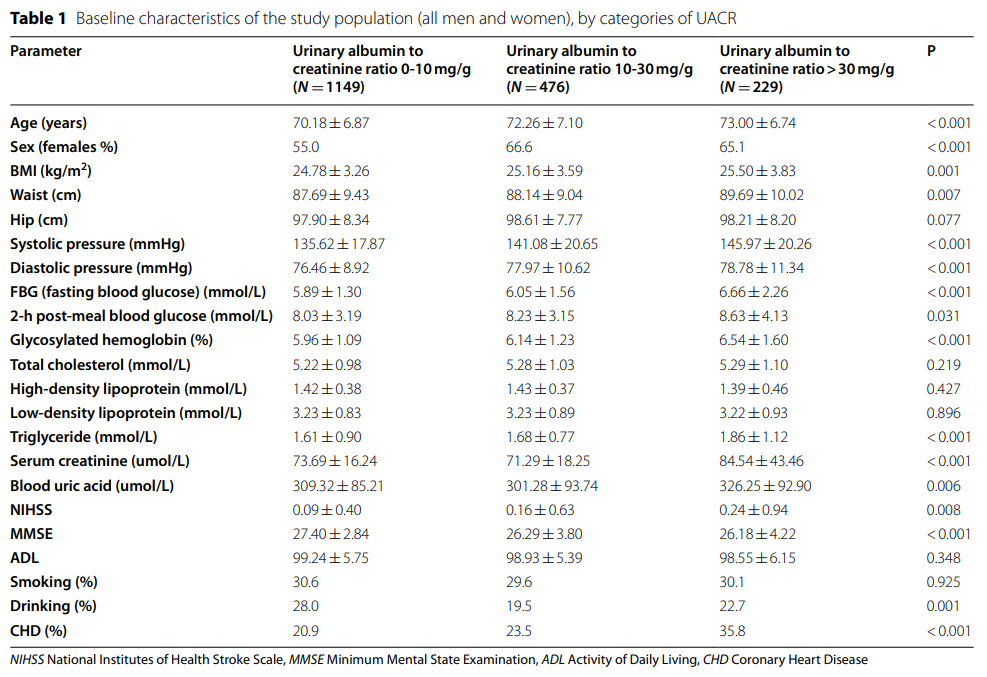
在1854个受试者中,有229人的UACR大于30 mg / g,蛋白尿的患病率为12.3%;1149人UACR < 10mg/g,占总数的62.0%;UACR为10mg /g ~ 30mg/g的患者有476人,占总人数的25.7%。妇女占人口的59.2%。表1显示了研究人群按研究组划分的基线特征。
1、全因死亡率
在平均9.87年(18,407.3人-随访年)期间,随访1854名受试者中340人死亡(185名男性和155名女性)。总人口、男性和女性的粗略全因死亡率分别为183.4/1000、99.8/1000和83.6/1000。男子的死亡率略高于妇女,这与该区域其他研究的结果一致。表2通过卡方检验显示根据尿白蛋白-肌酐比值比较三组全因死亡率。
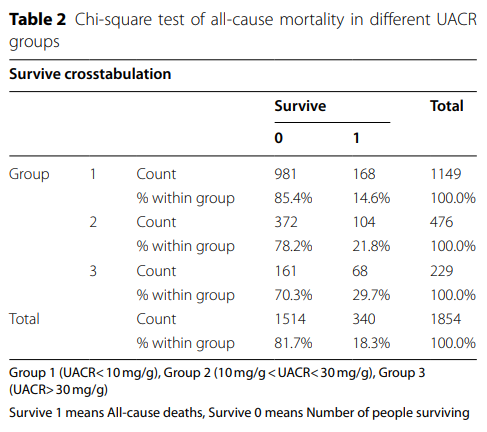
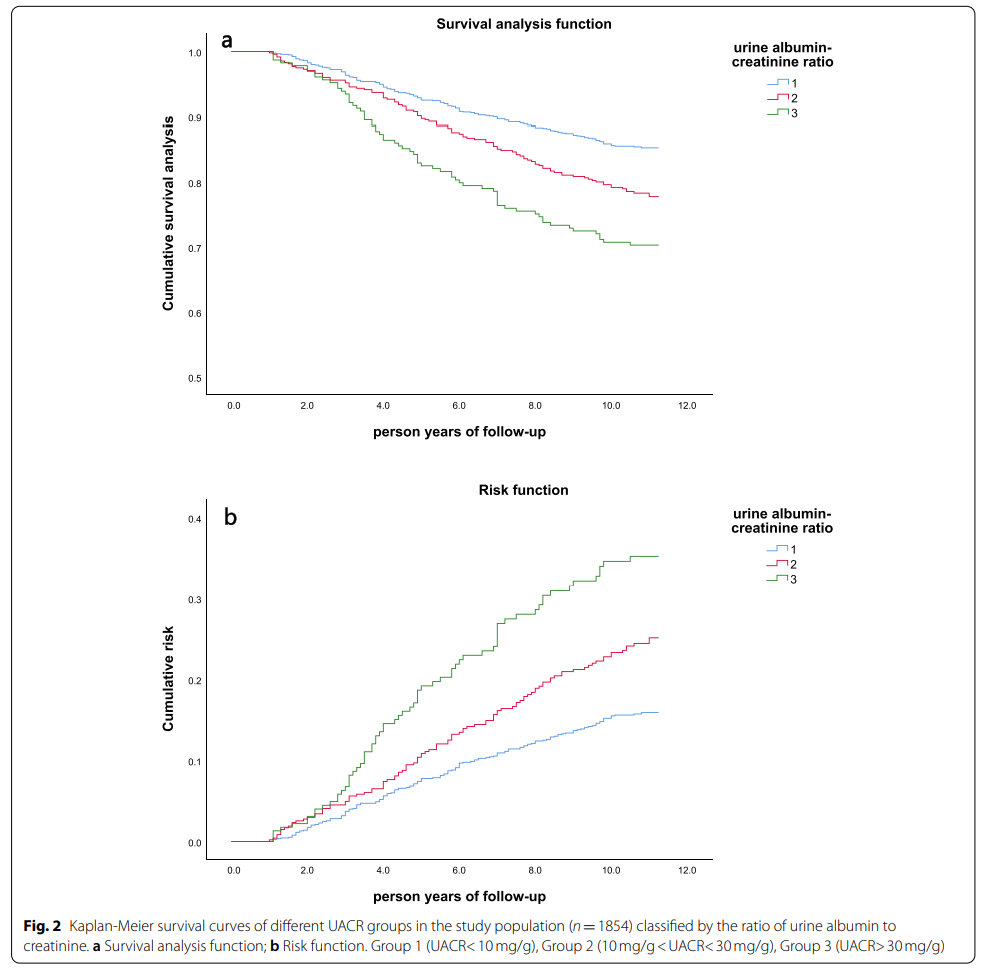
如表2所示,蛋白尿患者(第3组)的死亡率为29.7%,高于无蛋白尿人群。在尿蛋白正常的两组中,UACR高组(组2)的死亡率为21.8%,高于UACR低组(组1)。尿白蛋白与肌酐的比率越高,研究人群的死亡率就越高。采用Kaplan-Meier法和log-rank检验比较累积概率。 图2显示了不同尿白蛋白-肌酐比值的Kaplan-Meier生存曲线。UACR与全因死亡率之间存在显著的剂量-反应关系。研究人群的存活率随着UACR的增加呈显着下降趋势(p <0.001,通过Log-Rank测试)。从风险函数图中也可以看出,UACR越大,该组的累积生存风险就越大。
2、死亡风险
为了研究尿白蛋白- 肌酐比值对全因死亡率的影响,我们对数据进行了Cox比例风险模型拟合。除UACR外,回归分析中还包括以下可用于解释基线分析中全因死亡和组差异的变量:年龄,性别,身高,体重,BMI,腰围,收缩压,舒张压,甘油三酯,血肌酐,血尿酸,冠心病史,糖尿病史, 饮酒史。在调整上述可能影响生存的变量后,与组1(UACR<10 mg / g)相比,组2(10 mg / g <UACR<30 mg / g)和组3(UACR>30 mg / g)的全因死亡率显着升高。Cox比例风险模型用于分析多个变量,这使我们能够比较不同变量对所有原因导致的死亡的影响。通过风险比,将调整后的风险比绘制为UACR的函数,以及绘制特定协变量值的因果特定累积相关函数来汇总结果。
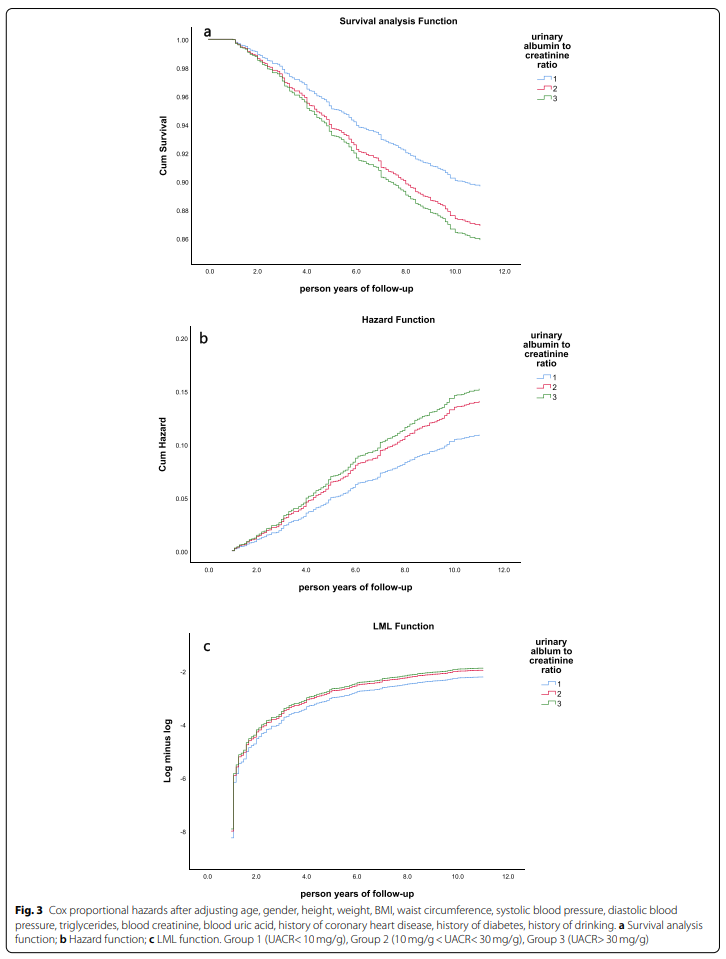
如图3所示,从生存分析曲线、风险曲线和LML函数可以看出,三组的生存率有显著差异(P<0.001),且UACR越大,组内死亡风险越大。在Cox比例风险模型中,以组1(UACR<10 mg / g)为参考,组2的风险比(HR值)是第1组的1.289倍(P = 0.048)。组3的风险比(心率值)是组1的1.394倍(P = 0.037)。由表3可知,高UACR患者的全因死亡风险低于低UACR患者的全因死亡风险。在Cox比例风险模型的每个影响因素中,与其他影响因素相比,UACR对全因死亡的影响较大。
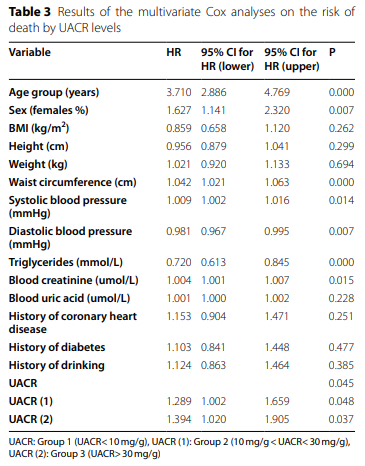
综上,本研究平均随访9.87年,总死亡率为183.4/1000。在 Cox 比例风险模型中,在调整了可能的混杂因素后,具有正常高值 UACR(组2)的患者的全因死亡率高于具有正常低值 UACR(组1)的患者 [HR 1.289, 95% CI 1.002 ~ 1.659]。蛋白尿患者(组3)的全因死亡率高于正常低值UACR(组1)[HR1.394,95%CI 1.020~1.905]。尿白蛋白与肌酐之比是社区人群中全因死亡的重要危险因素。即使在正常范围内(UACR<30 mg / g),正常高值(10 mg / g<UACR<30 mg / g)的人群全因死亡的风险也会增加。
本研究首次使用正常尿白蛋白与肌酐比值范围内的组来预测社区人群的全因死亡率,并进行10年的随访。过完只有在高血压和糖尿病患者中,医生才会关注患者的尿白蛋白与肌酐之比,因为许多研究表明蛋白尿与全因死亡独立相关。然而,在非糖尿病高血压人群和一般社区人群中,人们对尿白蛋白与肌酐的比例重视不够。通过本研究证据,在临床实践中,医生将更加关注UACR指标,在预测各种原因导致的死亡指标和标准方面有更多的选择。
原文来源:
Anhang Zhang, et al. The relationship between urinary albumin to creatinine ratio and all-cause mortality in the elderly population in the Chinese community: a 10-year follow-up study.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#全因死亡风险#
40
学习了
67
学到了新东西
54
学习了
64
#死亡风险#
34
学到新东西
61
新指标新启示!
61
学习了,谢谢
0
#高值#
32