周清教授:首个PD-1抑制剂头对头研究结果在2022 ASCO公布,中国创新药物彰显实力
2022-07-10 ASCO ASCO
CTONG1901研究结果为临床实践提供了重要的启示与指导意义。

近年来,免疫治疗为肺癌领域带来革命性突破。越来越多的研究证实无论是免疫单药还是联合治疗,其在晚期非小细胞肺癌(NSCLC)治疗中均发挥了重要的作用,以PD-1/ PD-L1抑制剂为主的免疫治疗已经成为NSCLC标准治疗之一。
随着新药的不断研发及普及,临床实践中可供选择的免疫药物激增。与此同时,新的问题也随之而来:不同免疫药物的疗效及安全性是否存在差异?为了探索这一问题,2019年,吴一龙教授团队发起了一项CTONG(中国胸部肿瘤协作组)1901研究,旨在对比信迪利单抗与帕博利珠单抗单药或联合化疗一线治疗晚期NSCLC的疗效与安全性。
在今年6月份召开的美国临床肿瘤协会(ASCO)年会上,首次公布了该研究期中分析数据。据研究者检索,CTONG1901研究是首个直接对比两种PD-1抑制剂之间疗效和安全性的头对头研究,引起了临床广泛关注。为此,特邀此项研究的主要研究者之一、广东省人民医院周清教授介绍CTONG1901研究设计,解读研究结果及其意义。
严谨设计,精准分层:CTONG1901敢为人先,掀起免疫药物“head-to-head comparison”新浪潮
周教授介绍,CTONG1901研究是一项开放标签、随机II期研究。该研究分为两个阶段,第一阶段,研究者设立了有效率的“门槛”,如果入组的少量患者经治疗后达到预设的有效率,该研究将进行扩展,入组更多患者进行第二阶段研究。
CTONG1901研究共入组了68例EGFR/ALK基因突变阴性的晚期NSCLC患者。根据PD-L1表达水平,患者被分为PD-L1 TPS(肿瘤比例评分)≥50%组与PD-L1 TPS<50%组。PD-L1 TPS≥50%患者以1:1的比例随机接受帕博利珠单抗(n=13)或信迪利单抗(n=14)单药一线治疗;而PD-L1 TPS<50%患者按照1:1的比例随机接受信迪利单抗联合化疗(n=20)或帕博利珠单抗联合化疗(n=21)一线治疗。该研究的主要终点为客观缓解率(ORR);次要终点为持续缓解时间(DoR)、疾病控制率(DCR)、安全性与耐受性、无进展生存期(PFS)及总生存期(OS)。
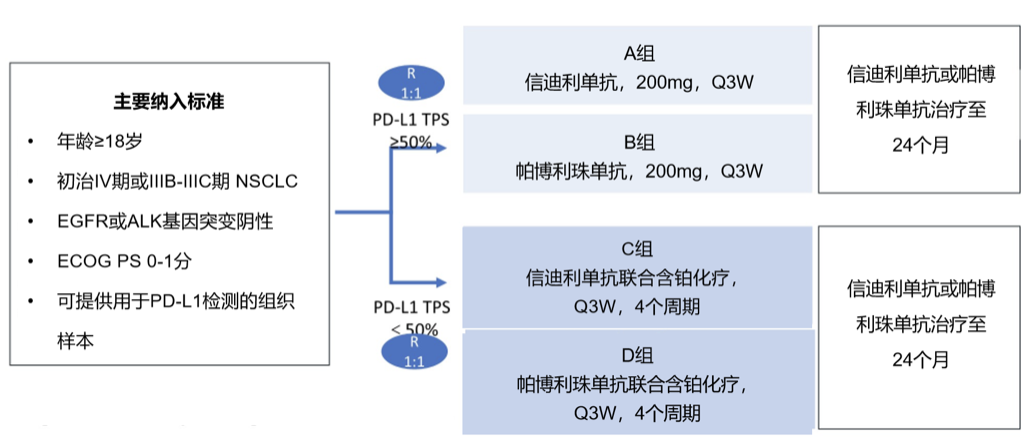
图1:CTONG1901研究设计
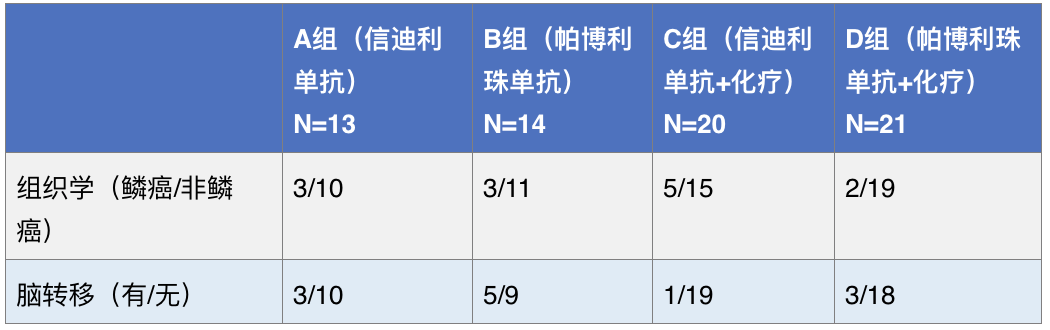
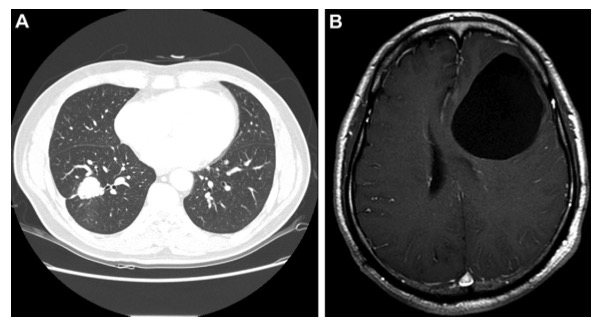
周教授指出,虽然CTONG1901研究规模较小,但其设计非常严谨。研究入组时,研究者根据不同组织学类型(鳞癌或非鳞癌)以及脑转移状态(有或无)对患者进行了分层,保证了影响因素的组间均衡性。基于研究设计的严谨性,不同影响因素在组间呈现平衡态势,为研究结果的解读奠定了良好的基础。
表1:患者基线特征简介
“能者立于不败之地”:信迪利单抗的疗效及安全性比肩帕博利珠单抗
CTONG1901研究结果显示,在研究第一阶段,信迪利单抗组与帕博利珠单抗组的ORR分别为57.1% vs 33.3%。信迪利单抗组4例患者取得部分缓解,达到预设终点,研究成功进入第二阶段。
在CTONG1901研究第二阶段,中位随访5.6个月的结果表明,在总体人群中,信迪利单抗治疗组与帕博利珠单抗治疗组的ORR分别为51.6% vs 30.3%。其中,信迪利单抗单药治疗组与帕博利珠单抗单药治疗组的ORR分别为38.5% 与28.6%;信迪利单抗联合化疗组与帕博利珠单抗联合化疗组的ORR分别为61.1%与31.6%。
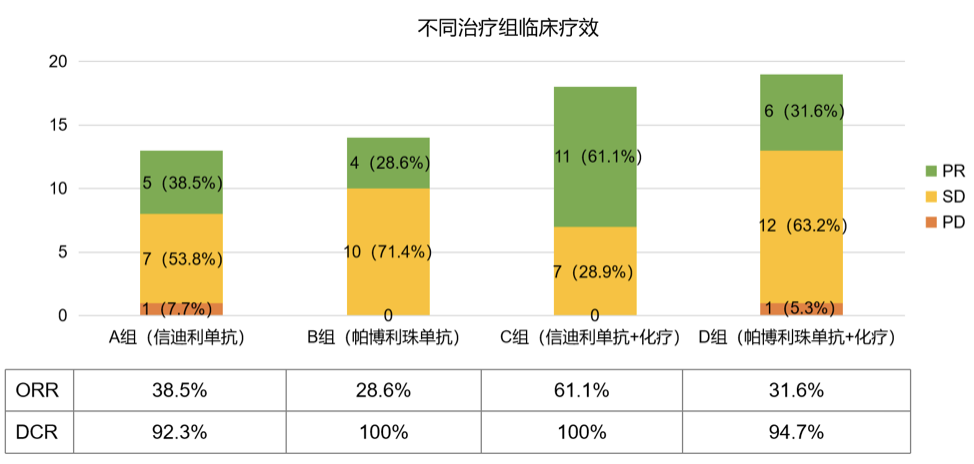
图2:CTONG1901研究疗效结果
周教授认为,虽然CTONG1901研究入组样本量较小,尚无法得出疗效差异结论,但两者相似的疗效同样让研究者感到欣慰。周教授特别提到,过去有人认为进口的药就一定是好的,但从CTONG1901研究结果不难发现,本土企业自主研发的创新药物——信迪利单抗取得了与进口药物帕博利珠单抗高度相似的疗效。
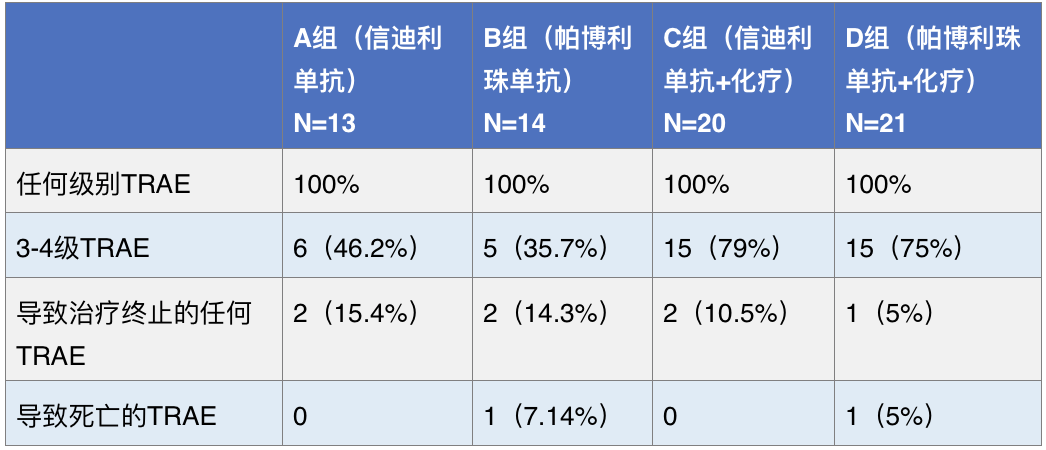
此外,在安全性方面,信迪利单抗治疗组与帕博利珠单抗治疗组任何级别和3-4级治疗相关不良事件(TRAE)相似。总体而言,信迪利单抗与帕博利珠单抗的疗效相当,安全性相似。
表2:CTONG1901研究安全性结果
CTONG1901研究结果为临床实践提供了重要的启示与指导意义。首先,其结果初步证实信迪利单抗与帕博利珠单抗均可作为临床较优的治疗方案,增加临床工作者选用国产免疫药物的信心。其次,该结果提示中国创新药物跑出“加速度”,未来有望实现从“跟跑”向“领跑”的重大转变。现阶段CTONG1901研究的生存数据尚未成熟,期待未来长期随访数据的进一步公布,以对临床治疗提供更多指导。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#新药物#
46
#头对头#
50
#ASC#
41
#抑制剂#
36
#研究结果#
45
#PD-1抑制剂#
41
#创新#
0