HAEMATOLOGICA:PET-CT状态对接受自体干细胞移植的复发性滤泡性淋巴瘤患者无进展生存期的影响
2022-05-23 网络 网络
复发或难治性 (R/R) 滤泡性淋巴瘤 (FL) 患者的最佳管理方法仍不确定。pet状态对接受自体干细胞移植的复发性滤泡性淋巴瘤患者有一定的预后价值,并可能有助于患者选择AutoACT。
复发或难治性 (R/R) 滤泡性淋巴瘤 (FL) 患者的最佳管理方法仍不确定。自体干细胞移植 (autoSCT) 被认为是适合年轻复发 FL 患者的标准选择。AutoSCT 与少数人非常持久的缓解有关,但也有显着的、公认的毒性。尽管在弥漫性大 B 细胞淋巴瘤和霍奇金淋巴瘤中建立了 autoSCT 前的 PET 状态,但在 FL 中没有数据。
一研究团队在一项国家、多中心、回顾性 BSBMTCT 登记研究中,根据卢加诺标准(完全代谢缓解 (CMR) 与非 CMR)在 172 名 R/R FL 患者中描述了根据 autoSCT 前 PET 状态的生存结果。autoSCT 后的中位随访时间为 27 个月(范围 3-70)。autoSCT 后所有患者的中位无进展生存期 (PFS) 为 28 个月(四分位距 23-36)。
AutoSCT时的年龄、性别、自上次复发后的月数、Karnofsky 体能状态或合并症指数 (HCT-CI) 与实现 CMR AutoSCT前 之间没有相互作用。
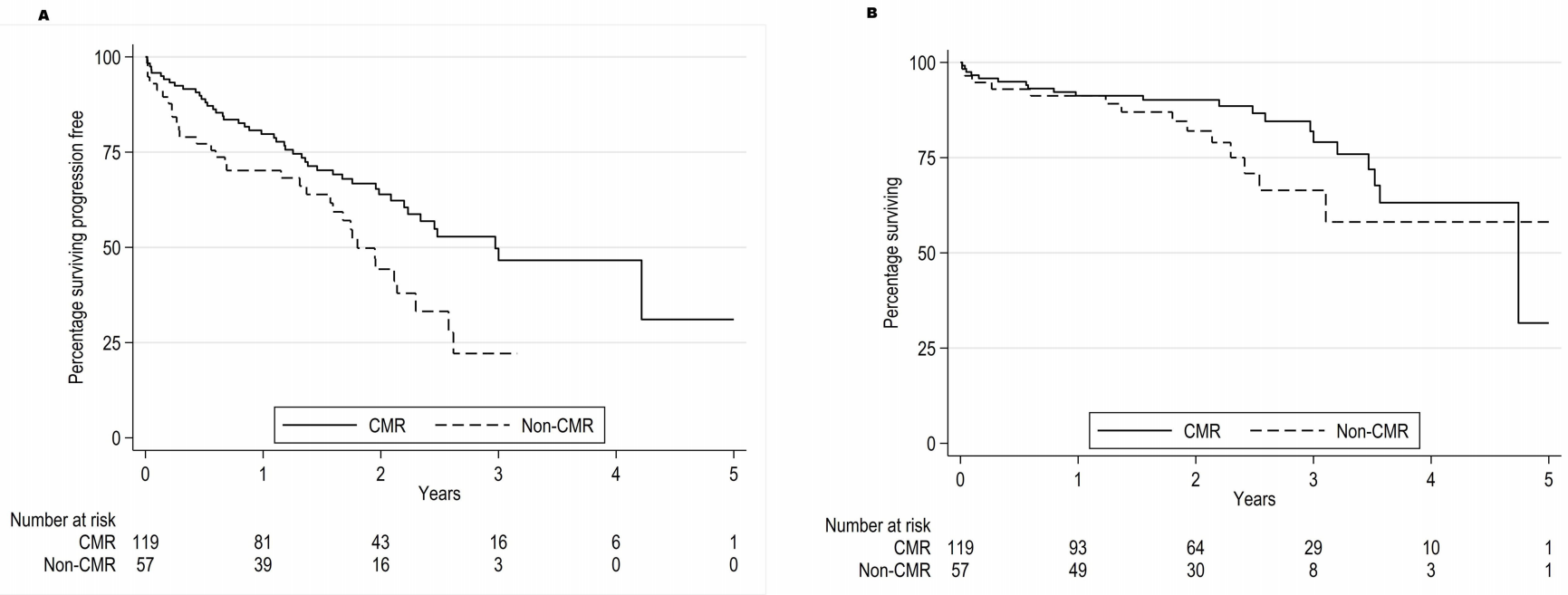
图1:自体干细胞移植前按pet状态进行移植后的生存率。图1A:自体干细胞移植前根据PET状态下的无进展生存期;图1B:根据自体干细胞移植前PET状态的总生存率
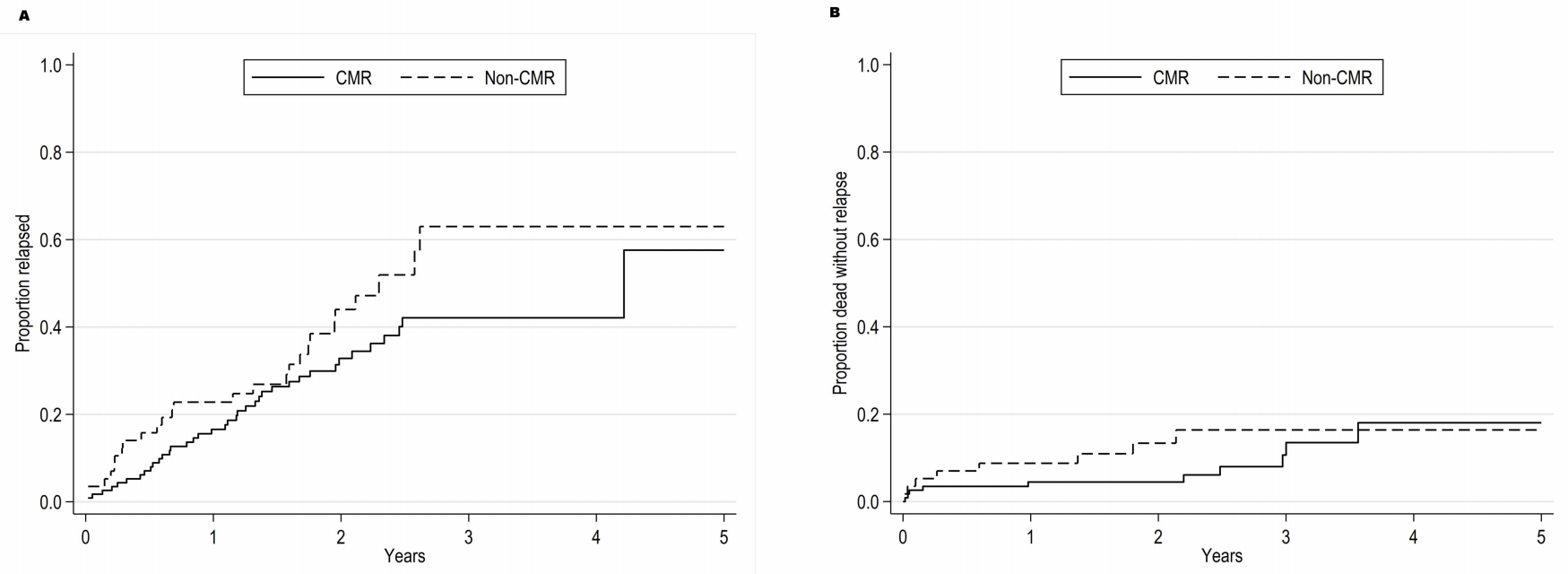
图2:根据pet-自体干细胞移植前状态的复发和非复发死亡率。图2A:自体干细胞移植前根据PET状态显示的复发率;图2B:自体干细胞移植前根据PET状态显示的非复发死亡率
115例(67%)CMR患者与57例(33%)非CMR患者(3年PFS 50% vs 22%, p=0.011)以及AutoSCT前的多维尔评分(连续变量1-5,HR1.32, p=0.049)均有较好的无进展生存期。经多变量分析,PET状态与AutoSCT后PFS(非CMR HR 2.02, p=0.003)、总生存期(非CMR HR 3.08, p=0.010)和复发风险(非CMR HR 1.64, p=0.046)独立相关。
总的来说,该研究的数据表明,pet状态对接受自体干细胞移植的复发性滤泡性淋巴瘤患者有一定的预后价值,并可能有助于患者选择AutoACT。
原始出处:
Eyre TA, Barrington SF, Okosun J, Abamba C, Pearce RM, Lee J, Carpenter B, Crawley CR, Bloor AJC, Gilleece M, Nicholson E, Shah N, Orchard K, Malladi R, Townsend WM. Impact of PET-CT status on progression-free survival for relapsed follicular lymphoma patients undergoing autologous stem cell transplant. Haematologica. 2022 May 19. doi: 10.3324/haematol.2021.280287. Epub ahead of print. PMID: 35586966.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#HAE#
48
#PE#
44
#复发性滤泡性淋巴瘤#
36
#复发性#
34
#细胞移植#
35
坚持学习
35
#滤泡性淋巴瘤#
38
#EMA#
27
#PET#
43
#生存期#
32