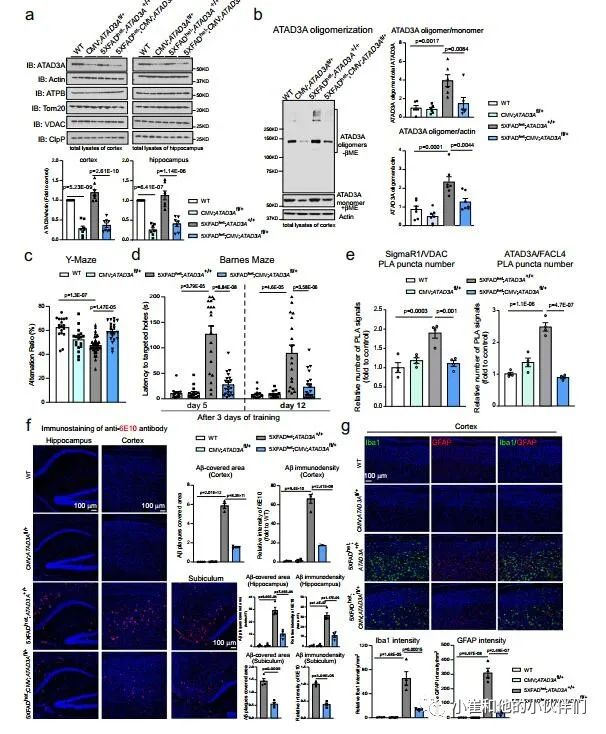
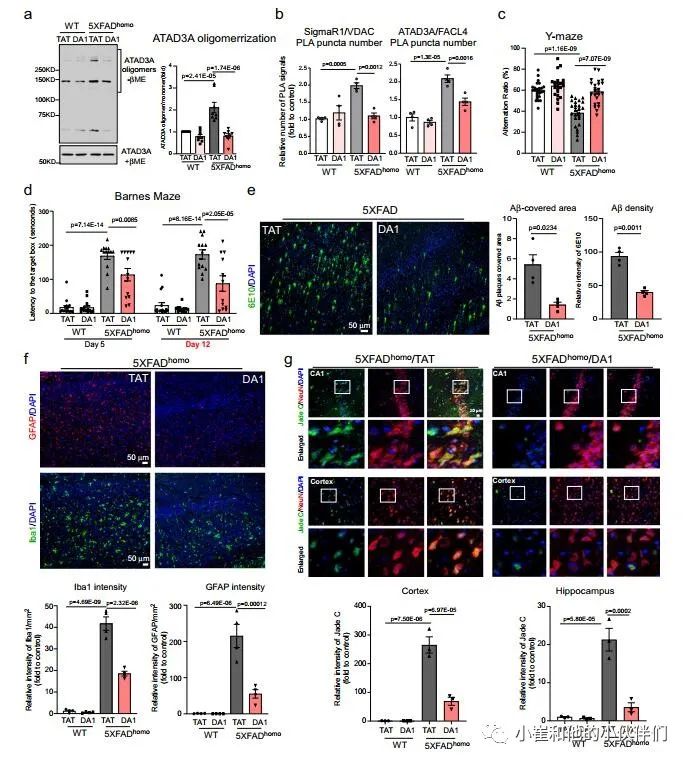
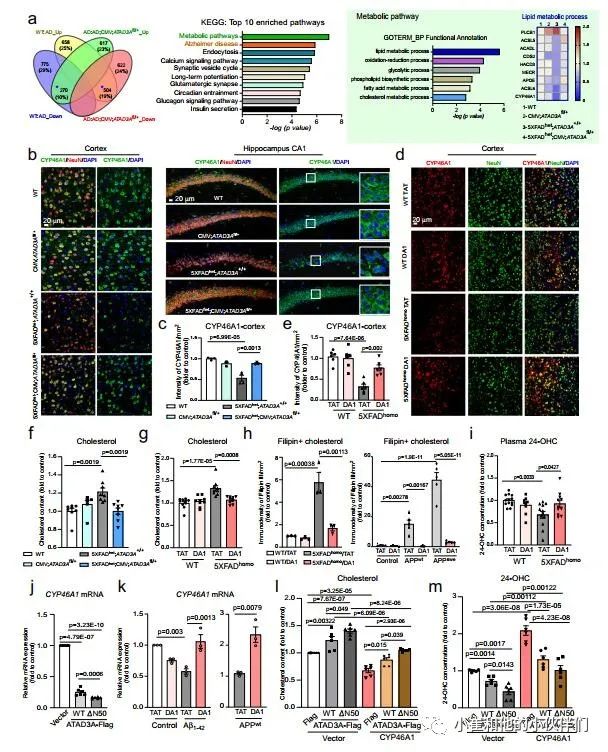
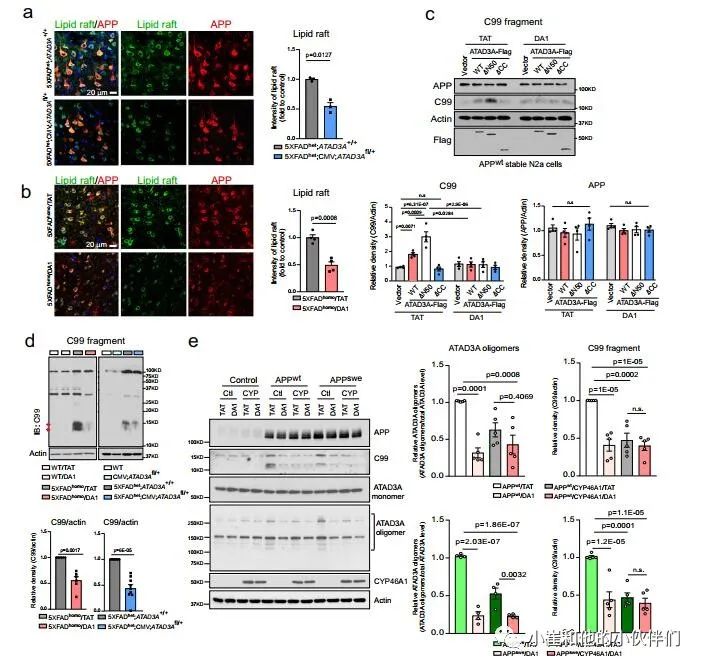
Nat Commun:ATAD3A寡聚化促进阿尔茨海默病模型的神经病理和认知损伤
2022-08-06 brainnew神内神外 网络
在 AD 病理学中观察到突触丧失,脑胆固醇代谢的破坏已被证明会导致突触丧失和随后的认知缺陷。















- END -
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#阿尔茨#
61
#Nat#
35
#认知损伤#
48
#阿尔茨海#
42
#COMMUN#
35
#损伤#
50
#ATA#
39
#阿尔茨海默#
38
#神经病#
56
#神经病理#
43