Human brain mapping:未用药强迫症患者局部脑神经活动的时间变异性
2021-06-26 MedSci原创 MedSci原创
强迫症患者CSTC回路内的区域性脑活动变异性增加,回路外区域变异性降低的特征性变化。特别地,强调CSTC回路外区域的功能障碍,如顶叶皮层和小脑在强迫症的病理生理学中起着重要作用。
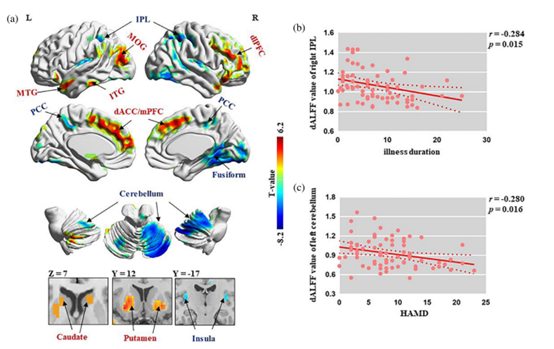
强迫症(OCD)是一种致残性精神疾病,一生的患病率约为2-3%。强迫症患者的特点是反复出现不想要的想法、图像或冲动(痴迷)和重复行为(强迫),这些都与实质性的全局残疾有关。尽管对与强迫症相关的神经功能缺损的探索取得了许多进展,但强迫症的确切神经机制仍不清楚。 强迫症(obsessive-compulsive disorder,OCD)表现为局部大脑活动的改变,表现为低频波动幅度(low-frequency frusion,ALFF) ,但这种局部神经活动的时变特征仍有待于进一步阐明。 最近,华西医院龚启勇团队发表研究文章,通过单变量和多变量分析,在一个相对较大的未用药强迫症患者样本中,研究内在脑活动的动态变化。 采用滑动窗口法计算dALFF ,并比较73例强迫症患者与年龄和性别匹配的健康对照(HCs)之间的差异。还利用多变量模式分析来确定 dALFF 能否在个体水平上区分强迫症患者和 HCs。 未用药强迫症患者与HCs之间的dALFF有显著差异 a)强迫症患者和HCS患者之间的显著区域比较。暖色/冷色表示强迫症组的dALFF值高于HCs的区域/低于HCs的区域。(b)病程与右侧IPL的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#mapping#
45
#脑神经#
38
#神经活动#
37
#human#
37
#变异#
27
#局部#
35