J Clin Oncol:Osimertinib用于携带EGFR罕见突变NSCLC患者的疗效和安全性
2020-01-05 QQY MedSci原创
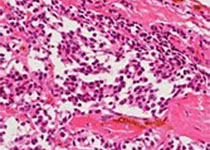
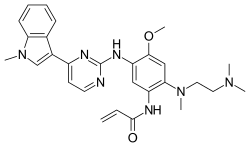
约10%的表皮生长因子受体(EGFR)突变阳性的非小细胞肺癌(NSCLC)患者携带罕见的突变。本文报告了osimertinib(奥斯替尼)用于携带罕见EGFR突变的NSCLC患者的有效性和安全性。本研究是一项在韩国开展的多中心、单臂、开放性的II期试验,招募除了携带EGFR 第19号外显子缺失、L858R和T790M突变以及第20号外显子插入突变以外的突变的病理明确诊断的转移性或复发性NSCLC患
本研究是一项在韩国开展的多中心、单臂、开放性的II期试验,招募除了携带EGFR 第19号外显子缺失、L858R和T790M突变以及第20号外显子插入突变以外的突变的病理明确诊断的转移性或复发性NSCLC患者。主要结点是每6周评估的客观缓解率。次要结点是无进展存活期、总体存活率、缓解持续时间和安全性。
2016年3月-2017年10月,共招募了37位患者,其中一位患者在治疗前退出研究。对于36位患者,中位年龄60岁,22位(61%)男性。61%的患者采用osimertinib作为一线治疗。最常见的突变为G719X(19例,53%),其次是L861Q(9例,25%)、S768I(8例,22%)和其他(4例,11%)。客观缓解率为50%(18例,95% CI 33%-67%)。中位无进展存活期为8.2个月(95% CI 5.9-10.5),总体存活期未达到。中位缓解持续时间为11.2个月(95% CI 7.7-14.7)。副作用有红疹(11例,31%)、瘙痒(9例,25%)、食欲减退(9例,25%)、腹泻(8例,22%)和呼吸困难(8例,22%),所有副作用可控。
本研究表明Osimertinib用于携带EGFR罕见突变的NSCLC患者中表现出良好的活性和可控制的副作用。
原始出处:
Jang Ho Cho, et al.Osimertinib for Patients With Non–Small-Cell Lung Cancer Harboring Uncommon EGFR Mutations: A Multicenter, Open-Label, Phase II Trial (KCSG-LU15-09) .Journal of Clinical Oncology. December 11, 2019.
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#EGFR罕见突变#
40
#Oncol#
37
#疗效和安全性#
37
#SCLC患者#
35
#NSCLC患者#
32
#osimertinib#
30
#罕见#
31
#GFR#
24
谢谢梅斯提供这么好的信息,学到很多
69
谢谢梅斯分享这么多精彩信息
60