Radiology:低剂量CT真的可靠吗?
2021-04-28 shaosai MedSci原创
胸部CT是CT成像中最常见的诊断任务之一。胸部CT能够显示高危患者的早期肺癌并降低肺癌死亡率,同时也可用于肺转移病灶的显示并为进一步的外科或药物治疗提供影像学参考依据。
胸部CT是CT成像中最常见的诊断任务之一。胸部CT能够显示高危患者的早期肺癌并降低肺癌死亡率,同时也可用于肺转移病灶的显示并为进一步的外科或药物治疗提供影像学参考依据。尽管胸部CT为临床常规使用的影像学工具,但胸部CT用于检测不确定性肺结节的辐射剂量差异很大。如果没有明确的良性形态学发现,则该肺结节被分类为不确定性肺结节。
美国国家肺癌筛查试验对于平均大小的肺结节使用了低剂量的胸部CT技术,其有效管电流时间乘积为20–30 mAs,从而产生了约1.5 mSv的有效辐射剂量。实施小剂量胸部CT的挑战主要包括观察者之间存在差异的可能性以及识别纯磨玻璃或混合磨玻璃(即亚实性)结节的困难。最近的一项系统分析显示,与滤波反投影(FBP)相比,迭代重建(IR)改善了低剂量胸部CT的图像质量。但也有研究表示,对于低对比度病变(CT值与解剖背景相似的病变),IR在较低辐射剂量下保持观察者诊断性能的能力有限。
近日,发表在Radiology杂志的一项研究比较了低剂量胸部CT与常规剂量胸部CT对5mm以上的不确定性肺结节的检测效果,为临床在保证图像质量的情况下尽可能降低患者的辐射剂量提供参考意见,为临床选择最适宜的胸部CT扫描条件提供数据支持。
本研究回顾性地收集了2013年11月至2014年4月期间83例患者(120 kV, 70质量参考mAs [QRM]) 83次常规胸部CT检查的CT投影数据。作为参考的不确定性肺结节由两位胸部放射科医师进行鉴定。通过使用经过验证的噪声插入,对5个低剂量数据集进行滤波反投影(FBP)或迭代重建(IR;30 QRM FBP, 10QRM IR, 5 QRM FBP, 5 QRM IR, 2.5 QRM IR)。由另外三名胸部放射科医生对肺结节进行画圈,对直径大于等于5mm的不确定性肺结节的可信度进行评级,并对图像质量进行分级。使用JAFROC优点图(FOM)和非劣效界限-0.10,在每个结节的基础上进行分析。
本研究共纳入42位患者(平均年龄51±17岁;21男21女)共66个不确定性肺结节(平均大小8.6 mm±3.4[标准差];亚实性结节21例)。与常规剂量CT的FOM相比(大小特异性剂量估计,6.5 mGy±1.8;FOM, 0.86[95%置信区间:0.80,0.91]),除了2.5 QRM IR外,FOM在所有低剂量配置中的表现都不差。在70 QRM时,对亚实性结节的敏感性为60%(范围,48%-72%),而在5 QRM或更低剂量时,无论是否使用IR,敏感性均显著下降(P < 0.05)。诊断图像质量随剂量降低而降低(P < .001),在5 QRM时成像质量较好(P < .05)。
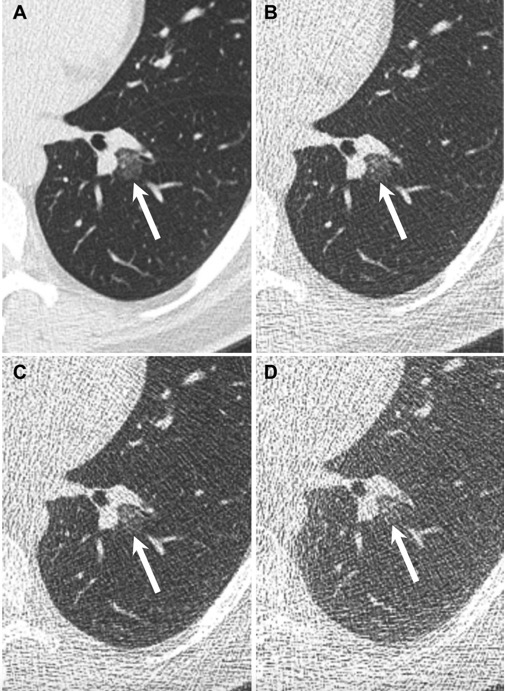
图1 44岁男性,胸部轴位CT表现为左肺下叶一个14.8毫米的亚实性结节(箭头)。(A)自动曝光控制设置70 QRM FBP,三位胸部放射科医生均在该图像上发现结节;(B)10 QRM IR,只有一位阅读者发现结节;(C) 5 QRM IR和(D)2.5 QRM IR,没有阅读者发现结节。值得注意的是,在C和D所显示的低剂量水平下,很难显示结节的磨玻璃部分。
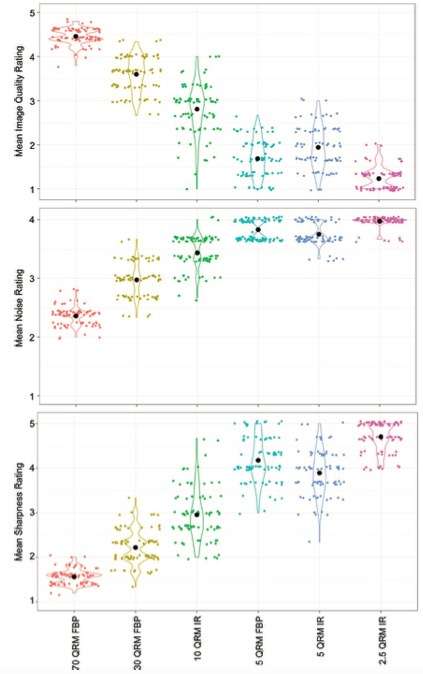
图2 散点图显示了常规(70质量参考mAs [QRM])和低剂量配置的图像质量指标。在对所有比较进行Tukey调整后,低剂量配置显著降低了总体诊断图像质量,同时增强了图像噪声并使所有两两比较的图像锐利度降低。在5-QRM剂量水平下,与滤波反投影(FBP)相比,迭代重建(IR)显著改善了三个图像的所有质量指标。横轴上黑点表示各剂量水平和重建组合的图像质量评分均值。
总而言之,为显示大于等于5mm的不确定性肺结节,胸部CT的辐射剂量水平可以比美国国家肺癌筛查试验中使用的剂量有限度地降低。本研究发现,极低辐射剂量将导致相当比例的亚实性不确定性肺结节无法清晰显示。同时在极低剂量下,迭代重建可改善主观图像质量,但不能改善阅读者的诊断性能。本研究结果提示,在不影响图像质量的前提下可在限制范围内小幅度的减少使用剂量,不能为追求过低的辐射剂量而影响进一步的诊断,这将本末倒置!
原文出处:
Joel G Fletcher,David L Levin,Anne-Marie G Sykes,et al.Observer Performance for Detection of Pulmonary Nodules at Chest CT over a Large Range of Radiation Dose Levels.DOI:10.1148/radiol.2020200969
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











KSNKSNNZK.JMIS.NZO JS J
58
KHSIEB0.643.0934.
36
学习了
64
#Radiology#点击进入话题查看更多相关文章 或评论时插入话题加入讨论
73
#低剂量CT#
36
#低剂量#
30
点赞
54
点个赞
43
学习了,谢谢分享
49