JAMA Netw Open:长期使用降压药物与主动脉夹层患者晚期结局的关系
2022-05-11 MedSci原创 MedSci原创
主动脉夹层(Aortic Dissection)是主动脉腔内的血液从主动脉内膜撕裂处进入主动脉中膜,使中膜分离,沿主动脉长轴方向扩展形成主动脉壁的真假两腔分离状态。
主动脉夹层(Aortic Dissection)是主动脉腔内的血液从主动脉内膜撕裂处进入主动脉中膜,使中膜分离,沿主动脉长轴方向扩展形成主动脉壁的真假两腔分离状态。据数据统计,主动脉夹层每年发病率为十万分之一至二十万分之一,年龄为50~70岁,男性发病率高于女性。

目前,主动脉夹层通常采用长期的药物治疗,以减少主动脉壁的压力并防止主动脉扩张或破裂。研究显示,β-受体阻滞剂可降低主动脉疾病的主动脉扩张率。欧洲心脏病学会、美国心脏病学院/美国心脏协会和日本循环学会的指南推荐β-受体阻滞剂用于急性主动脉夹层的初始治疗。随着医学的发展,越来越多的研究将血管紧张素转换酶抑制剂(ACEI),血管紧张素受体阻滞剂(ARB)与主动脉夹层的治疗联系起来。
近日,发表在JAMA Netw Open杂志的一项研究显示,β-受体阻滞剂、ACEI或ARB的使用与长期治疗主动脉夹层的益处有关。

在这项回顾性队列研究中,研究人员使用台湾国家健康保险研究数据库,共纳入6978名首次确诊为主动脉夹层的成年患者,这些患者在2001年1月1日至2013年12月31日期间存活至出院,并在出院后的前90天内接受了ACEI、ARB、β-阻滞剂或至少1种其他降压药物的处方,进而对患者全因死亡率、主动脉瘤、心脑血管不良事件、住院再治疗和新发透析进行探讨分析。数据分析时间为2019年7月至2020年6月。
结果显示,在6978名总参与者中,其中3492名患者接受了β-受体阻滞剂,1729名患者接受了ACEI或ARB,1757名患者接受了其他抗高血压药物。与其他两组患者相比,β-受体阻滞剂组患者更年轻(平均[SD]年龄,62.1[13.9]岁vs ACEI或ARBs的68.7[13.5]岁,对照组的69.9[13.8]岁),且男性患者更多(2520[72.2%]vs ACEI或ARBs的1161[67.1%],对照组的1224[69.7%])。
在ACEI或ARB组中,药物性高血压的患病率最高(1039例[60.1%]),其次是对照组(896例[51.0%]),在β受体阻滞剂组中最低(1577例[45.2]) %])。与ACEI或ARB(309例[17])相比,接受主动脉夹层手术的患者更倾向于β受体阻滞剂(1134例[32.5%])]或其他抗高血压药物(376例[21.4%])。因主动脉夹层而接受手术的患者,开具β-受体阻滞剂(1134例[32.5%])的可能性高于ACEI或ARB(309例[17.9%])或其他降压药物(376例[21.4%])。
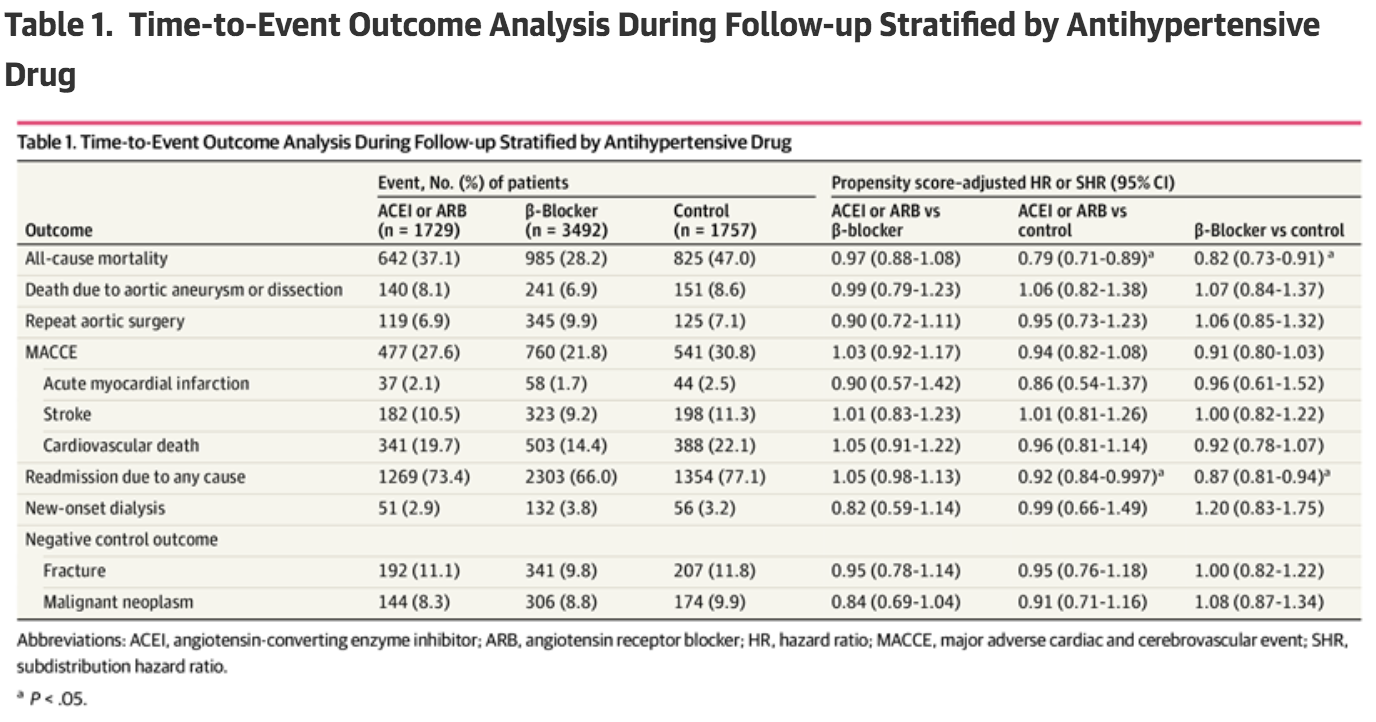
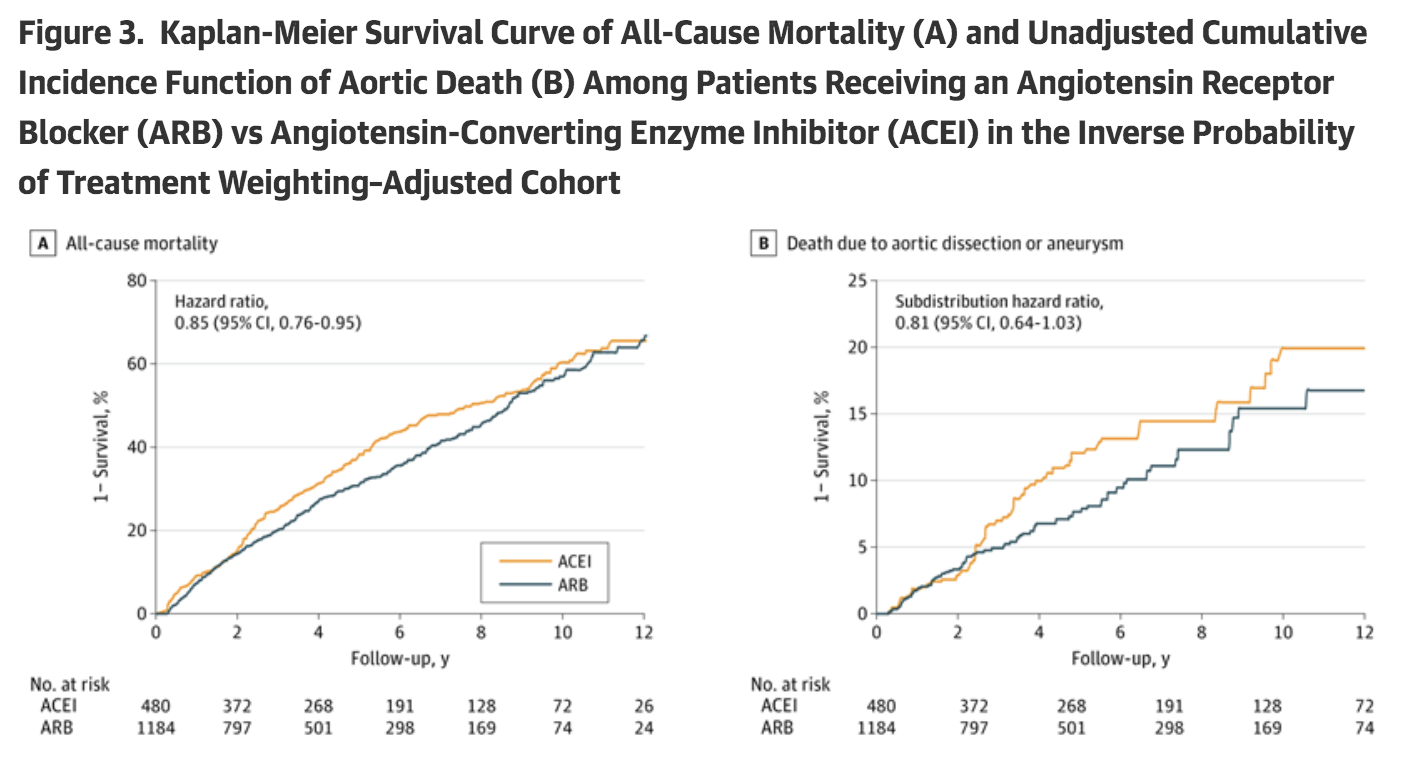
在调整多重倾向评分后,三组之间的临床特征均无显著差异,结局风险均无差异。ACEI或ARB组(亚分布危险比[HR],0.92;95%CI,0.84-0.997)和β-受体阻滞剂组(亚分布HR,0.87;95%CI,0.81-0.94)的全因住院再入院风险显著低于对照组。此外,ACEI或ARB组(HR,0.79;95% CI,0.71-0.89)和β-受体阻滞剂组(HR,0.82;95% CI,0.73-0.91)的全因死亡风险低于对照组。另外,ARB组的全因死亡风险低于ACEI组(HR,0.85;95% CI,0.76-0.95)。
综上,与对照组相比,使用β受体阻滞剂和ACEIs或ARBs可降低因任何原因导致的死亡和住院率。ARB治疗组的全因死亡风险低于ACEI治疗组。因此,ACEI和ARB疗法或可成为主动脉夹层长期治疗的替代方法。
原始出处
Shao-Wei Chen, MD, PhD1,2; Yi-Hsin Chan, MD3; Chia-Pin Lin, MD3; et al.Association of Long-term Use of Antihypertensive Medications With Late Outcomes Among Patients With Aortic Dissection.JAMA Netw Open. 2021;4(3):e210469. doi:10.1001/jamanetworkopen.2021.0469
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#长期使用#
51
#NET#
47
#PE#
43
#降压#
42
#主动脉#
52
#动脉夹层#
48
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
60
资料好
85