IBD: 使用抗 TNF 疗法可以降低炎症性肠病患者的结直肠癌发生率
2021-06-20 MedSci原创 MedSci原创
炎症性肠病 (IBD) 是一种慢性炎症性疾病,包括2种主要表型:克罗恩病(CD) 和溃疡性结肠炎 (UC)。
炎症性肠病 (IBD) 是一种慢性炎症性疾病,包括2种主要表型:克罗恩病(CD) 和溃疡性结肠炎 (UC)。在 IBD 治疗中,更有效药物的出现是减少手术干预的主要原因。众所周知,IBD患者多年的长期炎症会导致结直肠癌 (CRC) 的发病率高于一般人群,使得CRC 是公认的长期 IBD 患者的高发危险因素。但是,也有文献指出治疗IBD患者潜在的炎症可以降低CRC的风险。尽管在IBD患者中越来越多地使用生物制剂,但它们对结直肠癌发生的影响仍不清楚。因此,本项研究旨在探究生物制剂对 IBD 患者CRC的影响。

研究人员对一个由 1999 年至 2020 年间美国几家医院的电子病历组成的多中心数据库 (Explorys)收集了一组IBD的患者。然后进行了多变量分析,以调整包括药物和手术治疗在内的多种因素。

1999 年至 2020 年间,数据库中共有 62007510 名患者。其中,225090 (0.36%) 名患者患有克罗恩病,188420 (0.30%) 名患者患有溃疡性结肠炎。在使用多变量分析调整混杂因素后,IBD 患者更有可能发展为 CRC。在IBD队列中,接受抗TNF药物治疗的患者发生 CRC 的可能性较小;克罗恩病患者:优势比,0.69;95% 置信区间,0.66-0.73;P < 0.0001 vs 溃疡性结肠炎患者:优势比,0.78;95% 置信区间,0.73-0.83;P < 0.0001。
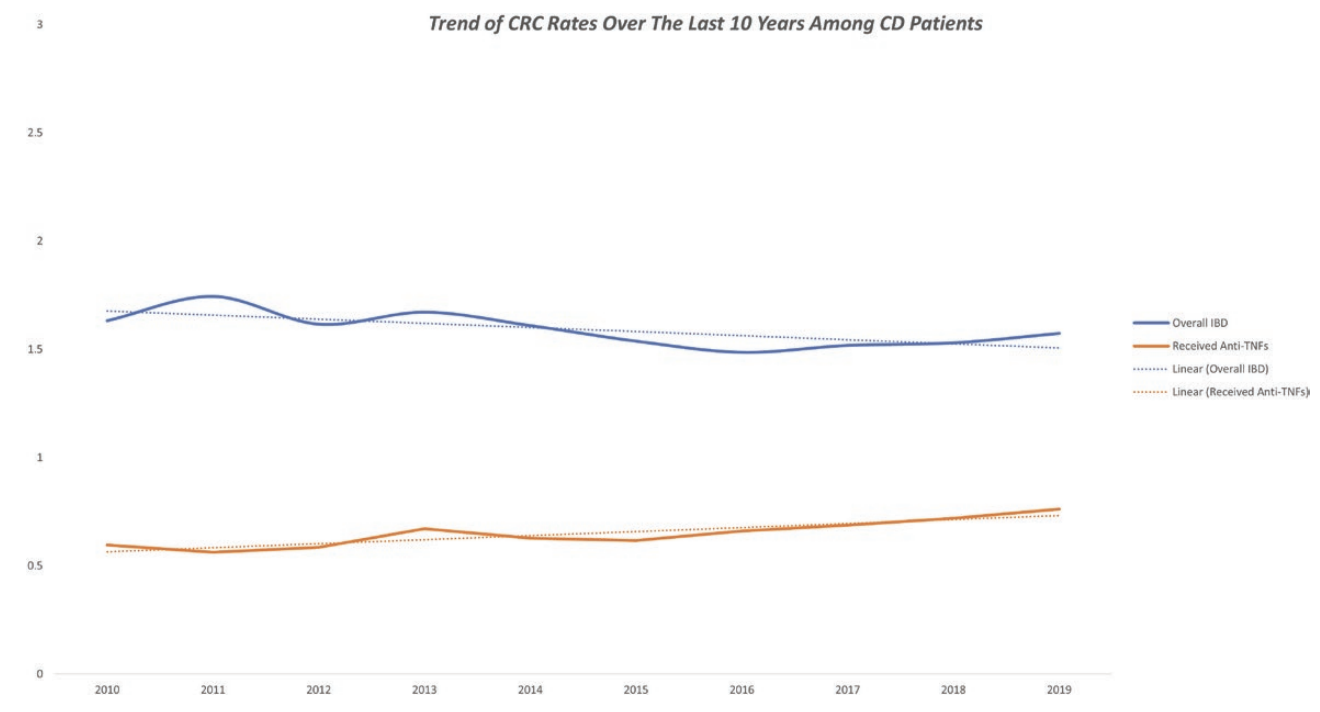
图:抗 TNF 疗法可以降低炎症性肠病患者的结直肠癌发生率
本项研究发现接受抗肿瘤坏死因子药物治疗的 IBD 患者发生 CRC 的可能性较小。需要前瞻性研究来评估抗肿瘤坏死因子药物是否通过炎症控制和粘膜愈合为 IBD 患者提供化学保护作用。
原始出处:
Motasem Alkhayyat. Et al. Lower Rates of Colorectal Cancer in Patients With Inflammatory Bowel Disease Using Anti-TNF Therapy. Inflammatory Bowel Diseases.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#发生率#
44
谈癌色变
59
#IBD#
34
#TNF#
39
#结直肠#
41
#炎症性#
42
#炎症性肠病患者#
37