BMC Pulmonary Med:我国继发性肺泡蛋白沉积症多继发于肺结核和骨髓异常增生症?哪些原发疾病可能影响其预后?
2018-03-24 张冬梅、田欣伦 呼吸界
在国家重点研发计划(2016YFC0901502)和北京市科技项目(Z151100003915126)支持下,北京协和医院呼吸科徐凯峰和田欣伦教授团队「Secondary pulmonary alveolar proteinosis:a single-center retrospective study(a case series and literature review)」(继发性肺泡蛋白沉积
在国家重点研发计划(2016YFC0901502)和北京市科技项目(Z151100003915126)支持下,北京协和医院呼吸科徐凯峰和田欣伦教授团队「Secondary pulmonary alveolar proteinosis:a single-center retrospective study(a case series and literature review)」(继发性肺泡蛋白沉积症的单中心回顾性研究及综述)于2018年1月16日在BMC Pulmonary Medicine杂志发表。张冬梅为该文第一作者。
该项回顾性研究纳入北京协和医院2001年1月至2016年7月内确诊的继发性肺泡蛋白沉积症患者9位,并回顾已发表文献,对继发性肺泡蛋白沉积症患者的病因、预后进行了相应的统计分析。
肺泡蛋白沉积症(PAP)是以肺泡腔内过量的脂蛋白沉积引起气体交换障碍,造成进行性呼吸功能不全的肺部罕见病。PAP患病率约为百万分之3.7~6.2。根据发病原因,其可分为自身免疫性(原称原发性或特发性)、继发性和先天性3种类型,其中90%以上为自身免疫性,存在抗粒细胞-巨噬细胞集落刺激因子(GM-CSF)抗体。继发性PAP由其他疾病导致,患者血清抗GM-CSF抗体阴性。
在BMC Pulm Med发表的这项研究发现,继发性PAP(SPAP)与自身免疫性PAP在临床表现及预后上存在很大不同。
该研究的发现包括以下几个方面:
1、与发达国家报道的SPAP主要继发于血液系统疾病(约为69%),而感染性疾病所继发者仅占8%不同,本组9例SPAP患者中,4例继发于肺结核,继发于血液系统疾病5例。肺结核的高发是导致我国继发性PAP病因分布不同的一个重要原因。
2、PAP的影像学常见表现为弥漫性磨玻璃影伴有小叶间隔增厚,但是仅有1/3的SPAP患者CT上可见典型的小叶间隔增厚。
3、文献回顾164例继发性PAP患者,确诊年龄平均为45.0±14.8岁,男女比例1.2:1,其中34.1%继发于骨髓异常增生症,15.2%继发于慢性粒细胞白血病。
4、继发于血液系统疾病的继发性PAP预期生存期短,中位生存期仅14.95个月。5年存活率为28.7%;而继发于其他疾病的SPAP的5年存活率为65%。继发于肺结核的SPAP常可通过抗结核治疗治愈。
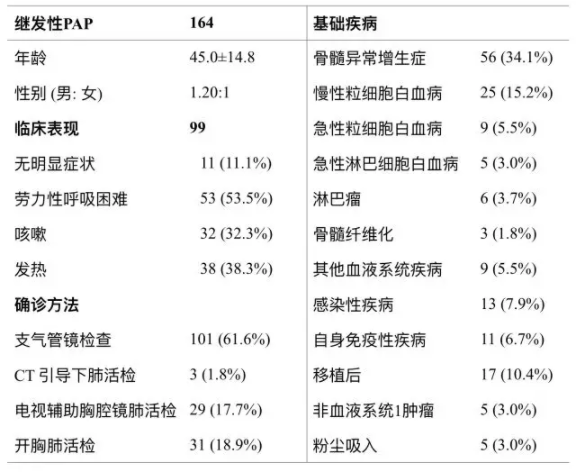
表1:164例SPAP特点
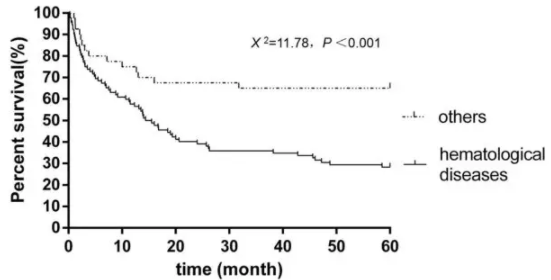
图1:不同基础病的SPAP患者的生存曲线
共132例继发性PAP患者具有生存资料,其中92例继发于血液系统疾病,中位生存期为14.95月,5年存活率为28.7%;40例继发于其他疾病,5年存活率为65%。
研究结果表明:我国继发性PAP多继发于骨髓异常增生症和肺结核。继发性PAP常发生在中年人,继发于血液系统疾病的患者预后差。若PAP患者CT上仅表现为磨玻璃影而无明显小叶间隔增厚,需要怀疑是否为继发性PAP。
原始出处:
Dongmei Zhang, Xinlun Tian, Ruie Feng, et al. Secondary pulmonary alveolar proteinosis: a single-center retrospective study (a case series and literature review). BMC Pulmonary Medicine. 25 January 2018.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#继发#
35
#BMC#
53
#继发性#
54
#pulmonary#
38
#结核#
44
#Med#
36
学习了谢谢分享.
0
学习了
63