PNAS:阻断钙通道有望成为治疗糖尿病的新策略!
2019-12-30 王昭月 生物探索
近日,瑞典Karolinska学院的研究人员发现并鉴定了一种钙通道——CaV3.1通道,它的过度激活会抑制胰岛素的释放,干扰葡萄糖稳态,进而导致糖尿病。这项研究发表在科学期刊PNAS上。
近日,瑞典Karolinska学院的研究人员发现并鉴定了一种钙通道——CaV3.1通道,它的过度激活会抑制胰岛素的释放,干扰葡萄糖稳态,进而导致糖尿病。这项研究发表在科学期刊PNAS上。
多种类型的电压门控钙通道(Voltage-gatedcalcium,CaV)存在于胰腺β细胞中,介导由血糖升高引起的Ca2+内流。其中,已有研究表明,CaV3通道介导的Ca2+内流参与了葡萄糖刺激的胰岛素分泌。CaV3.1(Voltage-gatedcalcium 3.1)通道可以调节正常大鼠和人类的小T型Ca2+电流,尤其在糖尿病条件下作用非常明显。
研究者构建了编码增强型绿色荧光蛋白-CaV3.1亚基(Ad-EGFP-CaV3.1)的重组腺病毒,它能有效地转导大鼠和人胰岛以及分散的胰岛细胞。以大鼠胰岛、人胰岛以及糖尿病大鼠为实验材料,研究了CaV3.1在糖尿病发病中的作用。结果发现,在大鼠胰岛中,CaV3.1通道表达的增加,选择性地损害了第一阶段葡萄糖刺激的胰岛素分泌。这种现象也存在于人类胰岛。同时,CaV3.1在体内糖尿病模型中的作用也得到了明确的证明。
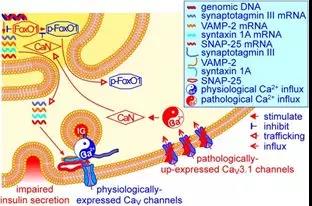
β细胞CaV3.1通道的高表达对胰岛素释放和葡萄糖稳态影响的模型
机制上,这是由于细胞质中磷酸化的FoxO1减少,FoxO1核保留增加,以及以CaV3.1通道和钙调蛋白依赖方式的合成素1A、SNAP-25和突触结合蛋白 III的减少。研究结果表明,胰岛中CaV3.1通道的表达升高可导致FoxO1介导的细胞外蛋白的下调,从而导致胰岛素分泌受损和葡萄糖稳态异常的糖尿病。这个因果关系确定了β细胞CaV3.1通道作为糖尿病治疗的潜在靶点。
原始出处:Jia Yu, Yue Shi, Kaixuan Zhao, et al. Enhanced expression of β cell CaV3.1 channels impairs insulin release and glucose homeostasis. PNAS. December 23, 2019
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#PNAS#
28
#阻断#
33
#新策略#
34
谢谢MedSci提供最新的资讯
55