Clin Gastroenterology H: 血液单核细胞产生的肿瘤坏死因子水平可用于预测炎症性肠病患者对英夫利昔单抗的反应
2021-03-28 MedSci原创 MedSci原创
抗肿瘤坏死因子(TNF)药物的出现彻底改变了炎症性肠病(IBD)患者的治疗模式,英夫利昔单抗是目前运用最广泛的抗肿瘤坏死因子(TNF)药物。
抗肿瘤坏死因子(TNF)药物的出现彻底改变了炎症性肠病(IBD)患者的治疗模式,英夫利昔单抗是目前运用最广泛的抗肿瘤坏死因子(TNF)药物。但是,并非所有患者都能受从英夫利西单抗药物中获得理想的疗效。临床上需要生物标志物来识别最有可能对治疗产生反应的患者。因此,本项研究探究了外周血单核细胞(PBMC)产生的肿瘤坏死因子(TNF)是否可以用作预测反应的标志物。

研究人员将过去6个月内未使用生物制剂治疗的41例IBD成人(平均年龄38岁; 21例男性; 21例克罗恩病和20例溃疡性结肠炎)进行了前瞻性研究。患者在德国柏林的一家医院接受了首次英夫利昔单抗治疗。研究人员在基线(首次输注之前)和6周(第三次输注)后收集了有关临床数据,C反应蛋白水平和超声检查结果(Limberg评分)的数据。在基线时研究人员收集了IBD患者和10位健康个体(对照)PMBC,并与脂多糖一起孵育。通过ELISA测定了细胞因子(TNF,白介素1 [IL1],IL6,IL8,IL10,IL12p70和IL22)的产生。主要观察终点是产生高水平或低水平TNF的PBMC患者的临床反应(Harvey Bradshaw指数评分降低2,或Mayo评分降低3)。
研究结果显示与无反应者相比,有反应者的疾病持续时间中位数较短(P = .018),而Limberg评分中位数较高(P = .021),基线PBMC产生的TNF(P = .049)和IL6(P = .028)明显高于未应答者。浓度为500 pg / ml TNF作为截止值时的模型预测药物治疗有效性的敏感度为82%,特异性为78%。在克罗恩氏病患者中,该临界值(500 pg / ml TNF)鉴定出的响应者具有100%的敏感性和82%的特异性。在多变量分析中,高于该水平的TNF水平与对英夫利昔单抗的反应独立相关(OR,16.2; 95%CI为1.8-148.7;P= .014)。
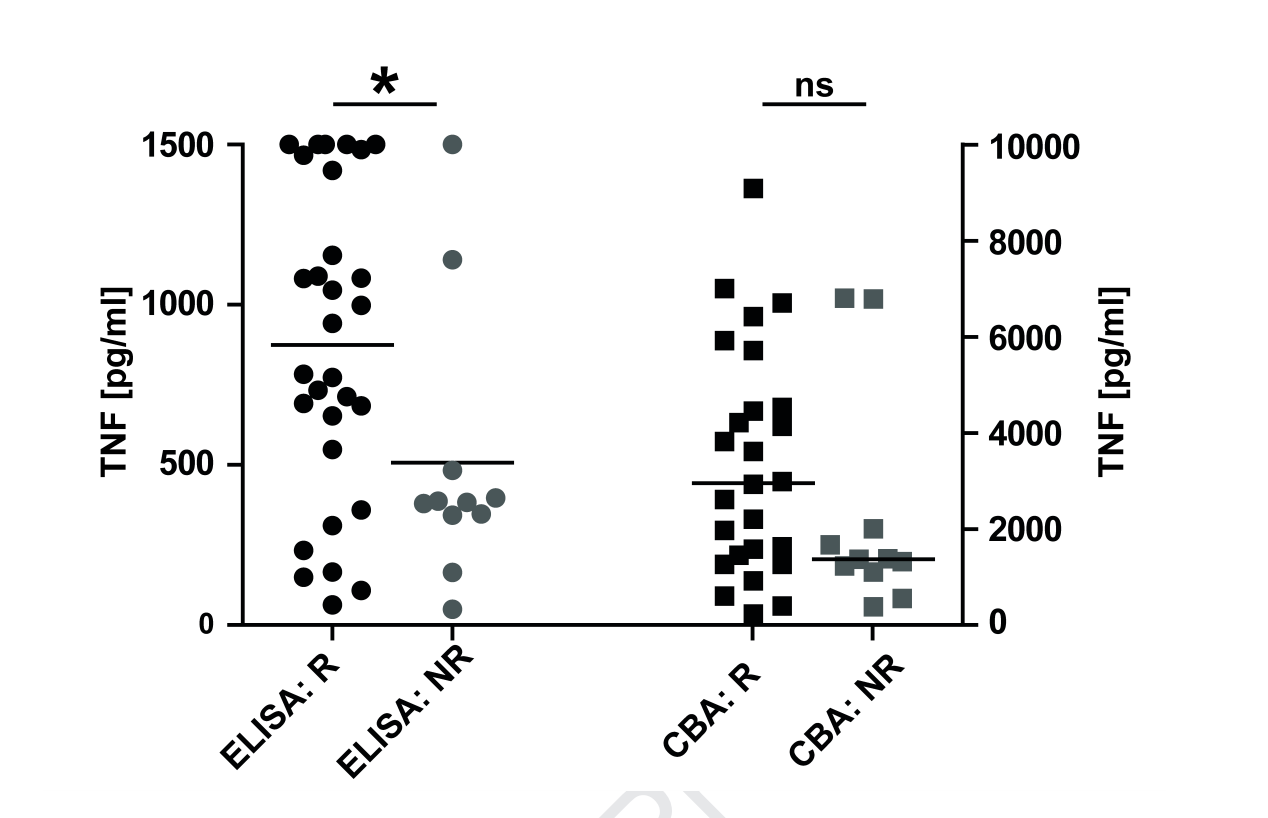
本项研究发现IBD患者的PBMC(特别是CD14+细胞)产生高水平的TNF可以鉴别出最有可能对英夫利昔单抗治疗产生临床反应的患者。在克罗恩氏病患者中,TNF的截断值为500pg/ml。
原始出处:
Bosse Jessen. Et al. Level of Tumor Necrosis Factor Production by Stimulated Blood Mononuclear Cells Can Be Used to Predict Response of Patients With Inflammatory Bowel Diseases to Infliximab. Clinical Gastroenterology and Hepatology.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Gastroenterol#
38
#AST#
30
#GAS#
27
#单核细胞#
34
#坏死#
26
#肿瘤坏死因子#
45
#Gastroenterology#
31
#炎症性#
29
#炎症性肠病患者#
0