Br J Cancer:多基因检测指导乳腺癌化疗的建议
2021-02-19 xiaozeng MedSci原创
乳腺癌作为女性中最常被诊断出的癌症。在包括英国在内的欧盟地区,在2018年里共有404,920名女性被诊断出患有乳腺癌,其中的98,755名患者死亡。
乳腺癌作为女性中最常被诊断出的癌症。在包括英国在内的欧盟地区,在2018年里共有404,920名女性被诊断出患有乳腺癌,其中的98,755名患者死亡。
其中激素受体(HoR)阳性(即ER(雌激素受体)阳性和/或PR(孕激素受体)阳性)、HER2(人类表皮生长因子受体2)阴性的乳腺癌患者约占西方国家诊断出的乳腺癌的70%。
在诊断之时,约有60%癌症的类型尚未扩散到淋巴结中,如果仅接受辅助内分泌治疗,约有15%的上述患者会在10年内复发。
因此,预测早期乳腺癌患者的复发风险和对化疗的应答对于辅助治疗测率的优化至关重要。因此,该研究旨在针对以下问题制定相应的医疗保健建议:在患有早期浸润性乳腺癌、激素受体阳性、HER2阴性的患者中,使用多基因检测是否能够指导辅助化疗的制定。
欧洲委员会乳腺癌倡议(ECIBC)旨在为乳腺癌的筛查和诊断提供基于证据的建议,ECIBC的指南制定小组(GDG)优先考虑了使用多基因检测的临床问题,以对HoR阳性、HER2阴性和淋巴结阴性或多达3个淋巴结阳性的浸润性乳腺癌患者进行辅助化疗指导。
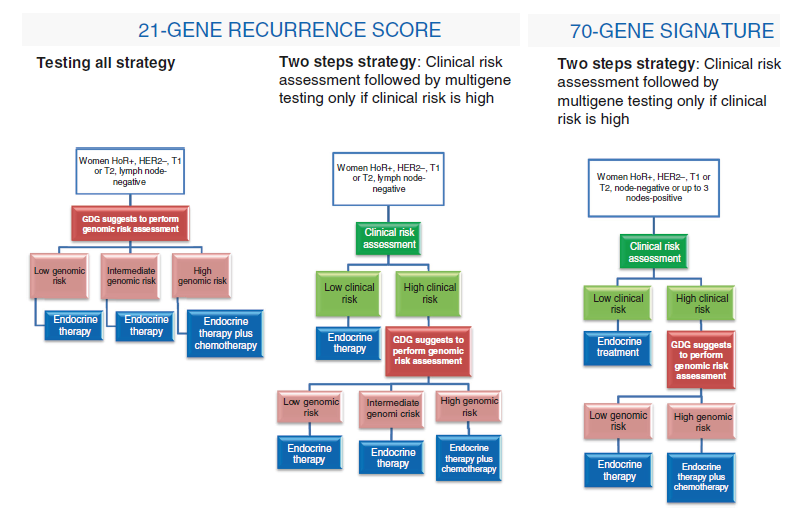
21-RS和70-GS相关流程示意图
在该研究中主要评估了四种多基因检测:21基因复发评分(21-RS)、70基因特征评分(70-GS)、50基因复发风险评分(PAM50-RORS)和12基因分子评分(12-MS)。
结果显示,在五项研究中(两项基因检测随机对照研究、两项随机对照研究二次分析以及一项来自观察性研究的汇总分析),并未鉴定出符合PAM50-RORS或12-MS的合格研究,且GDG未对这些测试提出相关建议。
因此,ECIBC GDG的建议如下:对于淋巴结阴性的女性推荐采用21-RS检测(有条件推荐,证据确定性极低),且根据临床特征,在复发风险较高的女性中其获益可能更大。对于临床风险高的女性推荐使用70-GS检测(有条件推荐,证据确定性低),并不推荐临床风险低的女性使用70-GS检测(推荐意见强,证据确定性低)。
原始出处:
Giorgi Rossi, P., Lebeau, A., Canelo-Aybar, C. et al. Recommendations from the European Commission Initiative on Breast Cancer for multigene testing to guide the use of adjuvant chemotherapy in patients with early breast cancer, hormone receptor positive, HER-2 negative. Br J Cancer (18 February 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#多基因#
40
#Br J Cancer#点击查看更多相关话题,或评论点击插入您喜欢的话题
69
已看,还可以。
50
很有指导意义
76
了解
79