Nat Commun:肿瘤内免疫异质性(ITH):肝细胞癌发生发展及肿瘤进化的标志
2021-01-18 xiaozeng MedSci原创
肝细胞癌(HCC)是一种异质性肿瘤,一般起源于慢性肝炎以及包括慢性病毒性肝炎、酒精中毒和脂肪肝疾病等多种病因。
肝细胞癌(HCC)是一种异质性肿瘤,一般起源于慢性肝炎以及包括慢性病毒性肝炎、酒精中毒和脂肪肝疾病等多种病因。由于该疾病的异质性特征,其靶向治疗的选择有限。HCC目前仍是全球癌症死亡的第三大主要原因。
目前最新的HCC相关免疫疗法仅能使对于PD-1免疫检查点阻断(ICB)有反应的患者的受益提高20%。因此,具有更高临床疗效的联合治疗成为当前免疫治疗的一个研究趋势。
基因组肿瘤内异质性(ITH)被认为是包括HCC在内的肿瘤发生发展以及进化的重要标志。然而,基于肿瘤浸润白细胞(TILs)的空间分布和表型的异质性程度,ITH在肿瘤微环境(TME)中的生物学和临床相关性尚不清楚。
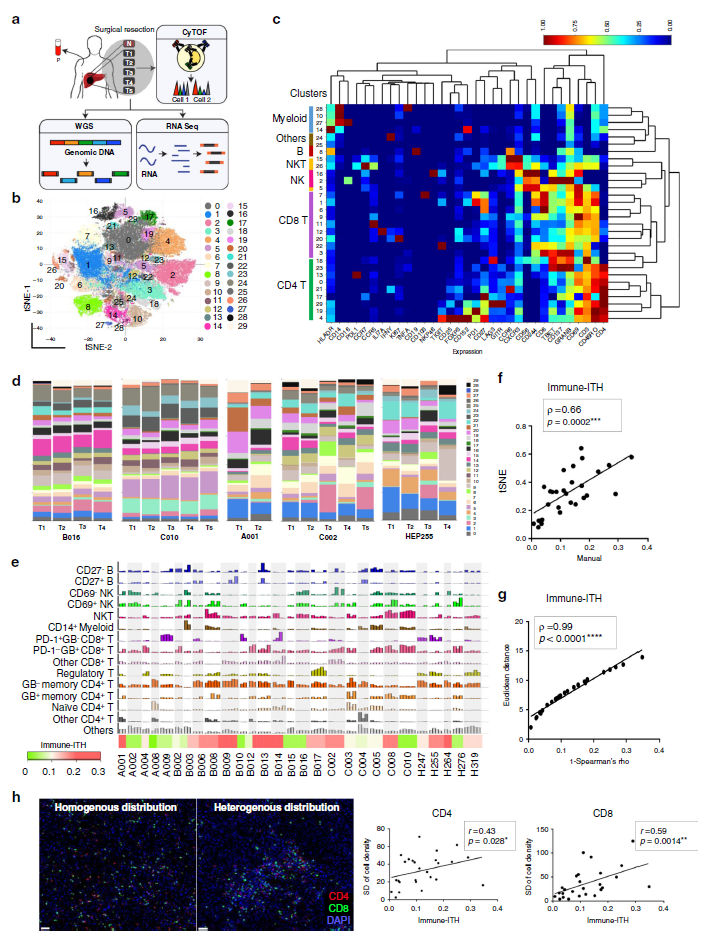
肝癌免疫环境中显著的肿瘤内异质性(ITH)
鉴于肝癌的致癌作用和疾病发生发展具有多步骤性质,因此研究和了解其免疫微环境的进化以及肿瘤基因组的进化显得尤为重要。
该研究旨在填补肿瘤ITH领域中的知识空白,并研究免疫ITH(immune-ITH)在肿瘤进化和疾病发展中的重要性。研究人员在多个肿瘤部位中发现了重要的空间和表型免疫ITH,并解释了其与HCC中肿瘤的演变和疾病发生发展的关系。
研究人员发现,免疫ITH与肿瘤转录组ITH、突变负担以及独特的免疫微环境相关。具有低免疫性ITH的肿瘤会经历更高的免疫选择压力,并能够通过人白细胞抗原杂合性的丧失和免疫编辑而引起免疫逃逸。
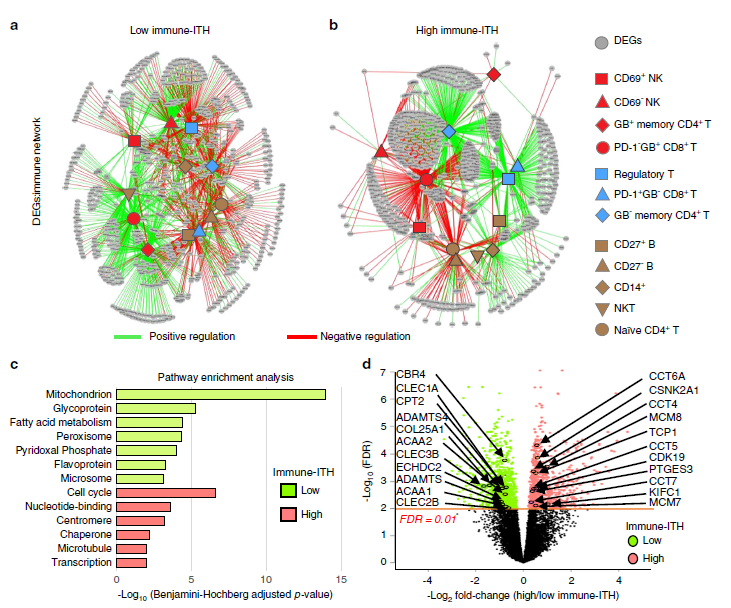
转录组免疫网络与肿瘤内免疫异质性相关(ITH)
取而代之的是,具有高免疫性ITH的肿瘤会演变为免疫抑制/耗竭的微环境。进一步的研究显示,免疫压力与免疫ITH的这种梯度关系是肿瘤的一种进化标志,其与疾病进展和免疫失活的免疫转录组网络密切相关。值得注意的是,高免疫性ITH及其转录组特征预示着HCC患者较差的临床预后。
综上,该研究结果显示,随着免疫ITH的增加,免疫格局得以重塑,而ITH的深入研究也为HCC的发生发展提供了肿瘤-免疫共进化方面的证据。
原始出处:
Nguyen, P.H.D., Ma, S., Phua, C.Z.J. et al. Intratumoural immune heterogeneity as a hallmark of tumour evolution and progression in hepatocellular carcinoma. Nat Commun 12, 227 (11 January 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞癌#
22
#Nat#
35
#发生发展#
30
#COMMUN#
36
#肝细胞#
31