The scientist
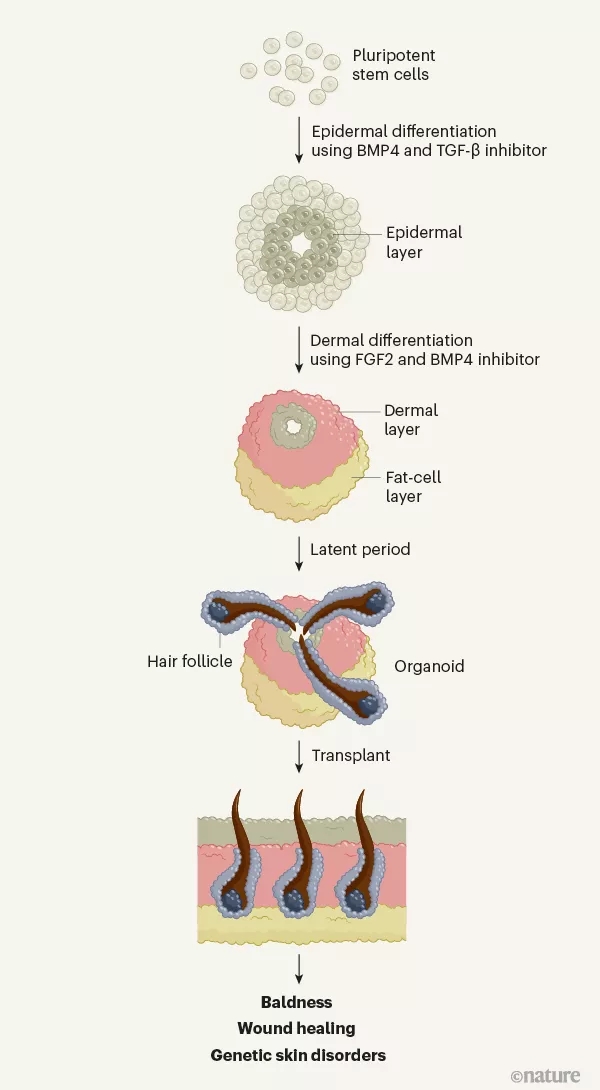
科学家们在过去十几年中已经证明,在实验室里由干细胞培养而来的小型类器官组织可以整合到许多器官中,包括小鼠的肝脏、肺等组织,用来修补损伤器官。
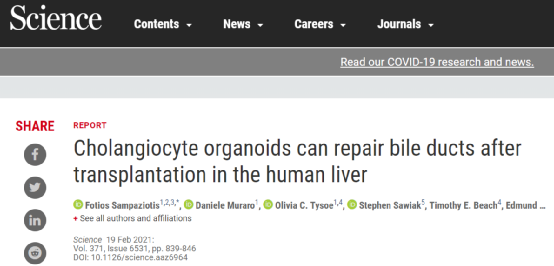
2月18日,在发表于《科学》(Science)杂志上的一项研究中,研究人员在人体组织中推进了这一方法,并证明由成人胆管细胞培养的“迷你胆管”可以移植到人体肝脏中。这为肝脏疾病的治疗提供了新方法,也为修复捐赠器官,以使更多的器官可用于移植铺平了道路。
DOI: 10.1126/science.aaz6964
在胆管损伤患者中,例如患原发性硬化性胆管炎的人,往往会胆管发炎,形成瘢痕组织,使胆管变窄和变硬,造成胆汁积聚,最终导致肝组织破坏。胆管疾病是导致70%的儿童及33%的成人肝脏移植的重要罪魁祸首。
来自英国剑桥干细胞研究所的研究人员曾在2017年发现,将从人类胆管细胞中提取的细胞移植到小鼠体内后,可以制造出类似胆管的结构。在今年的在这项新的研究中,他们试图将用这种类器官修复人类器官。
研究人员从捐献的人类胆管不同部位的胆管细胞中生成了不同类器官:肝内胆管,暴露在最低浓度的胆汁中;总胆管,胆汁浓度属中间水平;胆囊,储存浓缩胆汁。然后他们使用单细胞测序来检查基因表达。
细胞对胆汁中胆汁酸的暴露程度越高,编码保护其免于降解的蛋白质基因表达就越高。当研究小组将胆管细胞器官暴露于胆汁酸时,细胞增加了保护基因的表达。无论细胞最初来自肝脏的哪个地方,这种情况都会发生,这表明它们的基因表达是灵活的,并在很大程度上受环境的驱动。
为了证实这种灵活性,研究团队随后将这些类器官移植到胆管受到化学损伤的小鼠体内。结果显示,无论供体细胞移植到胆管何处,它们都能与宿主细胞融合,再生受损组织,并产生适当的蛋白质。得到类器官移植的小鼠存活了下来,而没有得到的对照组动物则很快死亡,这说明胆管细胞发挥了治愈作用。
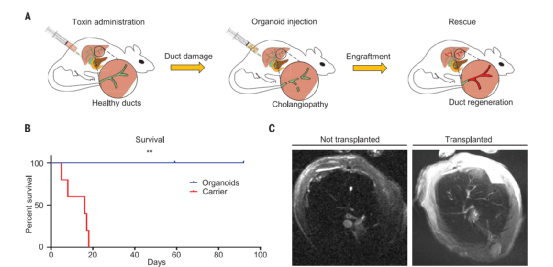
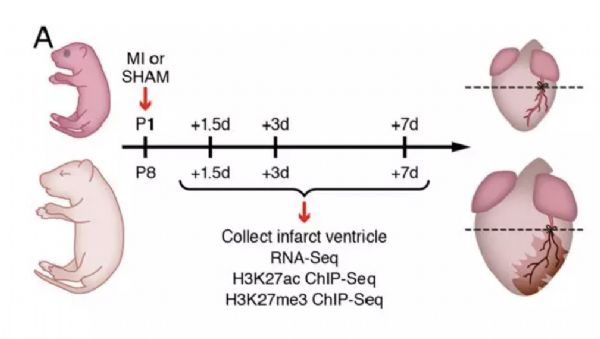
小鼠实验显示,类胆管细胞可在移植后挽救胆管病
然后,研究小组培养了一套新的人类器官组织,并将它们移植到三个捐赠的人类肝脏中(这些器官在体外人工系统中保持存活)。研究人员之所以使用这些肝脏,是因为移植手术前的常规评估显示,这些器官不够健康,无法捐给病人。同样的,试验结果发现,在人类肝脏中,移植的类器官修复了受损管道并恢复了它们的功能。

类胆管细胞移植入接受NMP的人肝脏
因此,这项研究证实基于细胞疗法可以用来修复受损的肝脏,这是胆管细胞生物学和再生医学方面的巨大进步。
鉴于供体器官的长期短缺,寻找修复受损器官的方法,甚至提供器官移植的替代方法是很重要的。类器官作为体外培养器官的微型版和简化版,无疑将加速多种器官和疾病的临床治疗。
类器官可能来自于组织中的一个或几个细胞、胚胎干细胞或诱导多能干细胞。自2010年初以来,这种培养和移植技术迅速提高,并被《科学家》(The scientist)评为2013年最大的科学进步之一。
科学家们已经学会了如何为细胞创造合适的环境,以便它们能够按照遗传学指令形成类器官结构。类器官的种类可能与体内不同组织和器官的种类一样多。迄今为止,科学家已经能够生产出类似于大脑、肾脏、舌、肺、肠道、胃和肝脏等类器官。
脑类器官
对于人类的大脑,这项技术为观察我们自身生物学中某些最难以捉摸的方面打开了一个窗口。当试图研究复杂的,固有的人类特征或疾病时,这一技术的应用显得尤为重要。比如当今一些最突出的神经精神疾病或神经发育疾病,例如精神分裂症或自闭症谱系障碍,就是独特的人类疾病,会影响整个人类基因组。
脑类器官包含了数以千计的细胞和多种脑细胞类型,它们以复杂的方式相互影响,使其成为研究神经精神病学或神经发育病理如何影响脑细胞的出色模型。
目前,有研究已经能够使用自闭症患者的类器官来显示与细胞增殖有关的基因调节异常。其他研究人员也已经使用类器官来观察寨卡病毒在早期胚胎发育过程中与小头畸形的关系,发现病毒通过驱动神经元产生细胞的过早分化来阻碍正常的大脑发育。其他人则在研究这些“正常”和“病态”的类器官对特定刺激的反应。
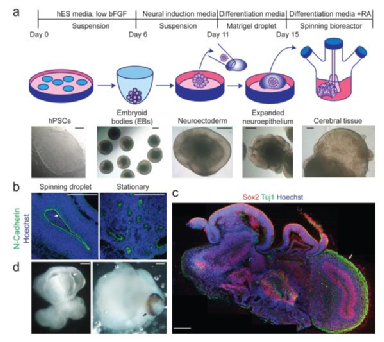
脑类器官培养系统
Cerebral organoids model human brain development and microcephaly.https://doi.org/10.1038/nature12517.
但是鉴于脑类器官可能会发展出知觉,具有类人的神经活动,有些科学家建议对该技术的进一步发展需要经过严格的监督程序。
肠类器官
肠类器官是指能概括胃肠道结构的类器官。迄今为止,肠类器官可由多能干细胞、胃肠道干细胞培养而来。一般来说,肠道类器官是研究肠道营养运输、药物吸收、胃肠道癌症和肠降血糖素激素分泌的有价值模型。例如,一项研究调查了胃癌患者转移性肿瘤人群背后的潜在基因改变,发现与患者的原发肿瘤不同,转移肿瘤中TGFBR2基因的两个等位基因都发生了突变。为了进一步评估TGFBR2在转移中的作用,研究者创建了敲除TGFBR2基因的类器官,由此发现TGFBR2活性降低会导致癌细胞的侵袭和转移。
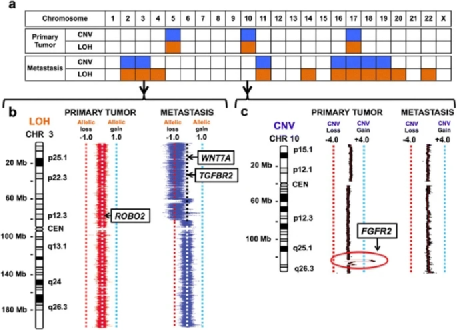
关键候选驱动因素与原发性胃癌卵巢转移的遗传差异
Metastatic tumor evolution and organoid modeling implicate TGFBR2as a cancer driver in diffuse gastric cancer.https://doi.org/10.1186/s13059-014-0428-9
舌类器官
舌类器官是指至少部分概括舌头生理方面的类器官。此前实验室可使用表达BMI1的上皮干细胞产生了上皮舌类器官,但这种类器官培养物缺乏味觉感受器。而如今科学家已经使用直接从分离的表达Lgr5-或LGR6的味觉干/祖细胞中成功地成功创建了这些味蕾类器官。
目前该领域创建的其他类器官还包括甲状腺类器官、胸腺类器官、睾丸类器官、上皮类器官、心脏类器官等等。
与异体器官移植相比,自体类器官移植减少了排异反应风险,与置入型医疗器械相比,其避免受磁场或黑客攻击的影响。在今年年初,苹果公司曾在最新支持文件中警告,不要将iPhone12和MagSafe配件太靠近置入式心脏起搏器等医疗设备。因为在1月份的一项测试中,医生发现iPhone12在靠近心脏起搏器时会使该设备失效,进入“暂停”状态。而采取类器官移植将避免这类尴尬。
DOI:https://doi.org/10.1016/j.hrthm.2020.12.032
总之,类器官技术为再生医学带来了巨大希望。目前临床上很多疾病都迫切需要增加器官供应或提供全器官移植的替代方法。在世界范围内器官捐献者一直是短缺的,只有有限数量的患者能从这种治疗中获益。而基于细胞的疗法可以提供一个有利的替代方案。
但这些新疗法的开发往往因缺乏适当的模型在人体中测试其安全性和有效性而受到阻碍和延迟,未来还需要进行更多临床试验加以验证。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













l,,kk,
76
#胆管#
28
学习
68
好
89
受益
73
认真学习了
67