EHJ:新发现!GWAS研究提示18个与左心房容积和功能相关的新位点
2021-11-27 MedSci原创 MedSci原创
左心房(LA)主要是作为从肺静脉进入心脏的血液储存室,对加强心室充盈很重要。
左心房(LA)主要是作为从肺静脉进入心脏的血液储存室,对加强心室充盈很重要。左心房(LA)容积和功能的变化与心脏功能受损、心律失常、中风风险和死亡率有关。左心房评估是标准超声心动图检查的一部分,传统上认为LA的变化是继发于其他心血管疾病。
然而,LA容积和功能变化背后的病理,以及与房颤(AF)、心力衰竭(HF)和中风风险的关系鲜为人知。人们对LA病理和心房组织越来越感兴趣,促使人们需要对心房心肌病进行定义。
LA的容积和功能如果受到损害,将对心血管的发病机制产生重大影响。为此,来自丹麦哥本哈根大学医院心脏病学专家旨在利用心脏磁共振成像数据研究LA容积和功能的遗传结构。结果发表在《欧洲心脏病杂志》。

研究人员使用了英国生物库——是一个大型的前瞻性人口研究中可用的表型和遗传数据。在35658个欧洲人的子集上,对五个容积和功能的LA变量进行了全基因组关联研究,这些变量是用机器学习算法生成的。
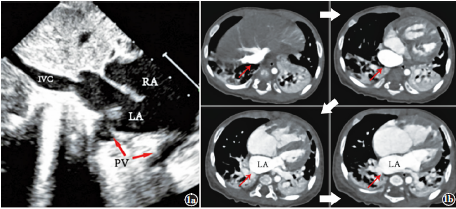
结果总共确定了18个新的遗传位点,这些位点映射到在心肌病(如MYO18B、TTN、DSP、ANKRD1)和心律失常(如TTN、CASQ2、MYO18B、C9orf3)中具有已知作用的基因。我们观察到LA体积和功能与中风之间的高度遗传相关性,这在LA被动排空分数方面最为明显(rg = 0.40,P = 4 × 10-6)。
为了研究心房颤动(AF)的遗传风险是否与明显的心房颤动之前的LA特征有关,研究人员制作了一个心房颤动的多基因风险评分。结果显示在没有房颤的参与者中,房颤的多基因风险与洛杉矶体积增加和洛杉矶功能下降有关[LAmax 0.25(mL/m2)/ SD,95%CI 0. 15;0.36);LAmin 0.21(mL/m2)/SD,95%CI 0.15;0.28);LA主动排空分数-0.35%/SD,95%CI(-0.43;-0.26)。

图形摘要
综上,该研究发现18个与LA体积和功能有关的遗传位点,并显示了几个对LA结构很重要的可信的候选基因的证据。
参考文献:
Genome-wide association study identifies 18 novel loci associated with left atrial volume and function, European Heart Journal, Volume 42, Issue 44, 21 November 2021, Pages 4523–4534, https://doi.org/10.1093/eurheartj/ehab466
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#新位点#
44
#左心房#
54
#新发现#
43
#GWAS#
73
#心房#
46