病例分享:双靶齐下的乳腺癌抗HER2治疗
2019-01-18 唐静 王先明 邸立军 肿瘤资讯
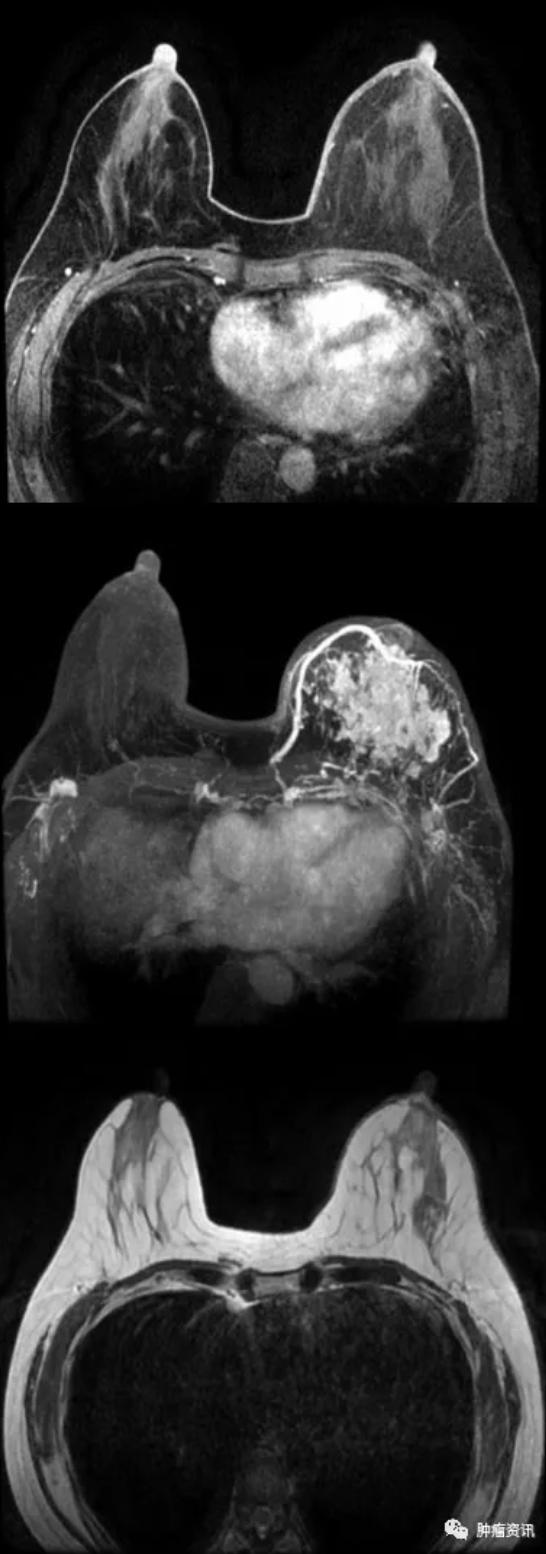
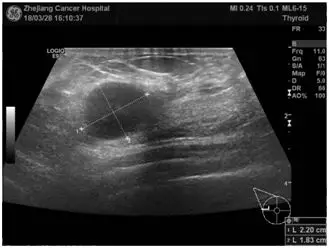
患者女性,48岁,围绝经期。2018年7月以“发现左乳肿物半年余”为主诉入院。既往体健,否认慢性病、传染病史。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#抗Her2治疗#
47
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。给点赞啦
96
谢谢分享,学习了
0
学习了
85
学习了长知识
84
学习了很有用不错
91
学习了,涨知识了!
28