Gut:中国研究发现暴露于替诺福韦母婴阻断治疗的胎儿长期安全性良好
2021-05-13 网络 网络
胎儿暴露于预防乙型肝炎母婴传播的富马酸替诺福韦酯(TDF)后,其身体、神经发育长期情况仍不明确。来自我国多中心的研究人员探究了替诺福韦治疗在妊娠晚期的安全性。
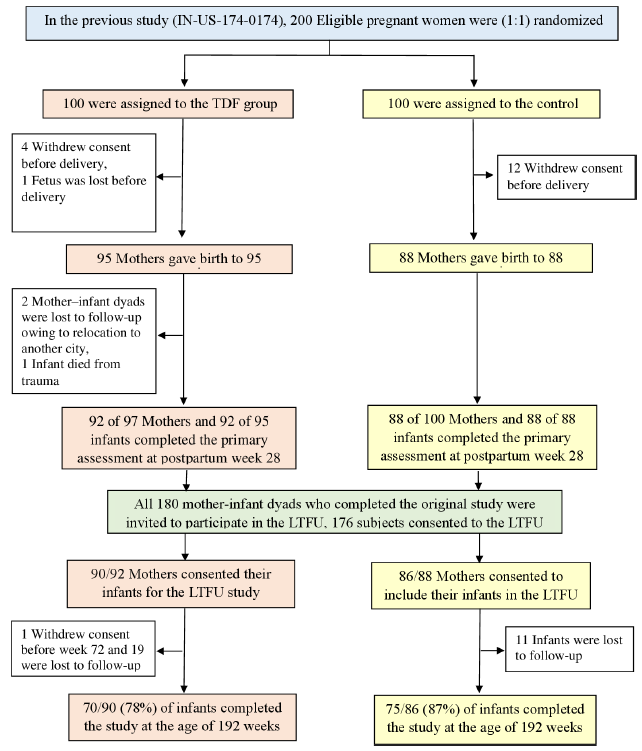
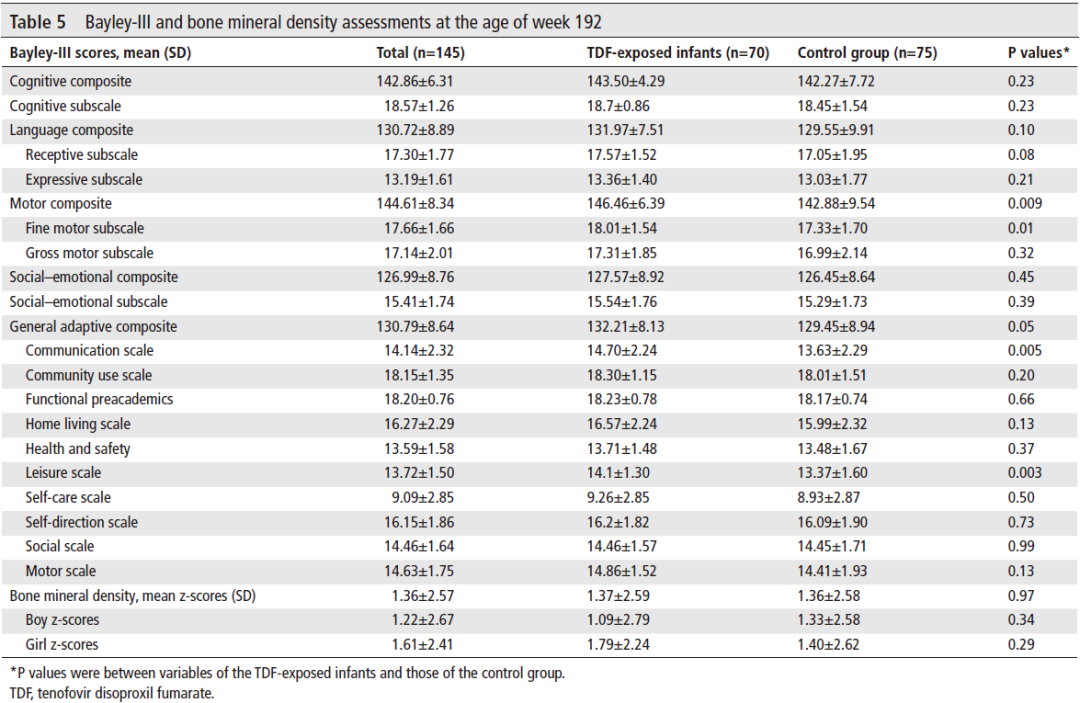
胎儿暴露于预防乙型肝炎母婴传播的富马酸替诺福韦酯(TDF)后,其身体、神经发育长期情况仍不明确。来自我国多中心的研究人员探究了替诺福韦治疗在妊娠晚期的安全性。 该研究团队先前开展的随机对照试验(IN-US-174-0174)样本被纳入此次长期随访(LTFU)研究。患慢性乙型肝炎的母亲被随机分配,在妊娠晚期接受或不接受替诺福韦治疗。使用Bayley-Ⅲ评估192周龄时婴儿的躯体生长或畸形、骨密度(BMD)和神经发育情况。 在180名符合条件婴儿中,176名婴儿入组,145名婴儿完成了长期随访(对照组:75名;替诺福韦治疗组:70名)。替诺福韦治疗组,胎儿接触替诺福韦的平均时间为8.57±0.53周。 在第192周时,两组的先天性畸形率相似。对照组和替诺福韦治疗组分别与国家标准比较,男孩的平均体重显著较高,而且在正常范围内。其他预定的结果(头围、身高、骨密度、认知、运动、社交情绪和适应行为测量)在组差异均有统计学意义。 胎儿暴露于替诺福韦的婴儿在第192周时身体生长、骨密度和神经发育正常。本研究为胎儿暴露于母体替诺福韦预防乙型肝炎传播的长期安全性提供了证据。 摘译自:PAN CQ, DAI E, DUAN Z, et al. Long-term safety of infants from mothers with chronic hepatitis B treated with tenofovir disoproxil in China[J]. Gut, 2021. 吉林大学第一医院感染病中心肝病科
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#阻断#
41
#研究发现#
27
#母婴阻断#
37
#长期安全性#
32
#替诺福韦#
35
#母婴#
35