JAMA:中国学者大发现!DEVT试验结果提示直接取栓非劣于桥接取栓!
2021-01-20 MedSci原创 MedSci原创
本研究结果有力支持跨过静脉溶栓,进行直接动脉取栓治疗,为急性卒中救治提供新策略,为卒中管理指南更新提供新证据,为减少个人和医保费用支出,减少家庭和社会经济负担提供新方法。
2020年10月29日是第15个 “世界卒中日”,后者是由世界卒中组织于2004年呼吁设立的。去年的主题宣传片中强调,每4个人有至少1人在一生中会发生卒中,我们的目标就是,不要成为这个人。
卒中,通常称为“中风”,是全球第二大死因,仅次于心血管疾病(CVD)。而中国是全球卒中负担最高的国家,终生风险高达39.3%。卒中具有发病率高、死亡率高、致残率高、复发率高“四高”的特点。目前,我国带病生存者高达1300万。
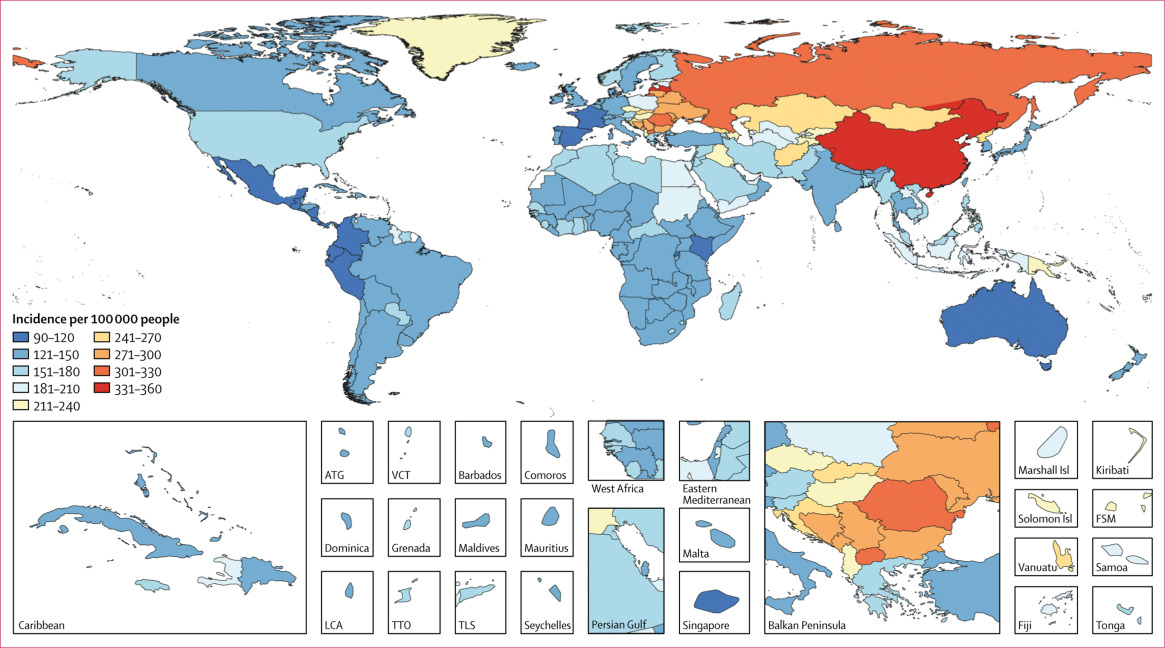
根据中国卒中学会联合中国疾病预防控制中心最新发布的《中国卒中报告2019》显示,仅2018年,我国因卒中死亡人数为157万人,约占全球卒中死亡人数的1/3,占居民总死亡率的22.3%,也就是说我国每五位死亡者中就有一人死于脑卒中。因此,卒中已成为我国成年人致死和致残的主要原因,同时也是过早死亡和疾病负担的首位原因。
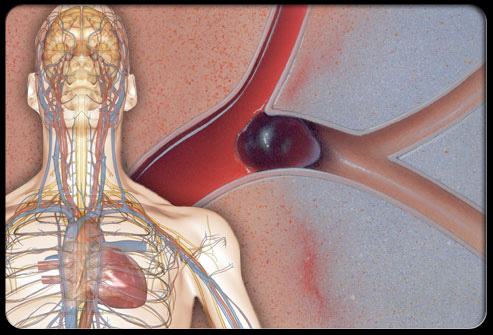
急性缺血性脑卒中再灌注治疗的早期目标是恢复已缺血但尚未梗死脑区的血流。远期目标则是降低脑卒中相关致残率和死亡率,改善结局。目前,明确有效的再灌注治疗方案包括静脉用阿替普酶、静脉用替奈普酶和机械取栓。
然而,目前有关脑卒中救治领域中的临床关键问题,即继发于大血管闭塞并符合溶栓条件的缺血性卒中患者能否跨过静脉溶栓直接进行动脉取栓治疗一直是一个尚未有满意答案的临床问题。如果能够跨过静脉溶栓、直接进行动脉取栓,则可以通过减少救治环节、加快救治速度,更快实现闭塞血管再通,从而有效降低卒中的致死率和致残率。因此,这不仅是脑卒中救治领域中的重大科学问题,同时也是重大社会经济问题。
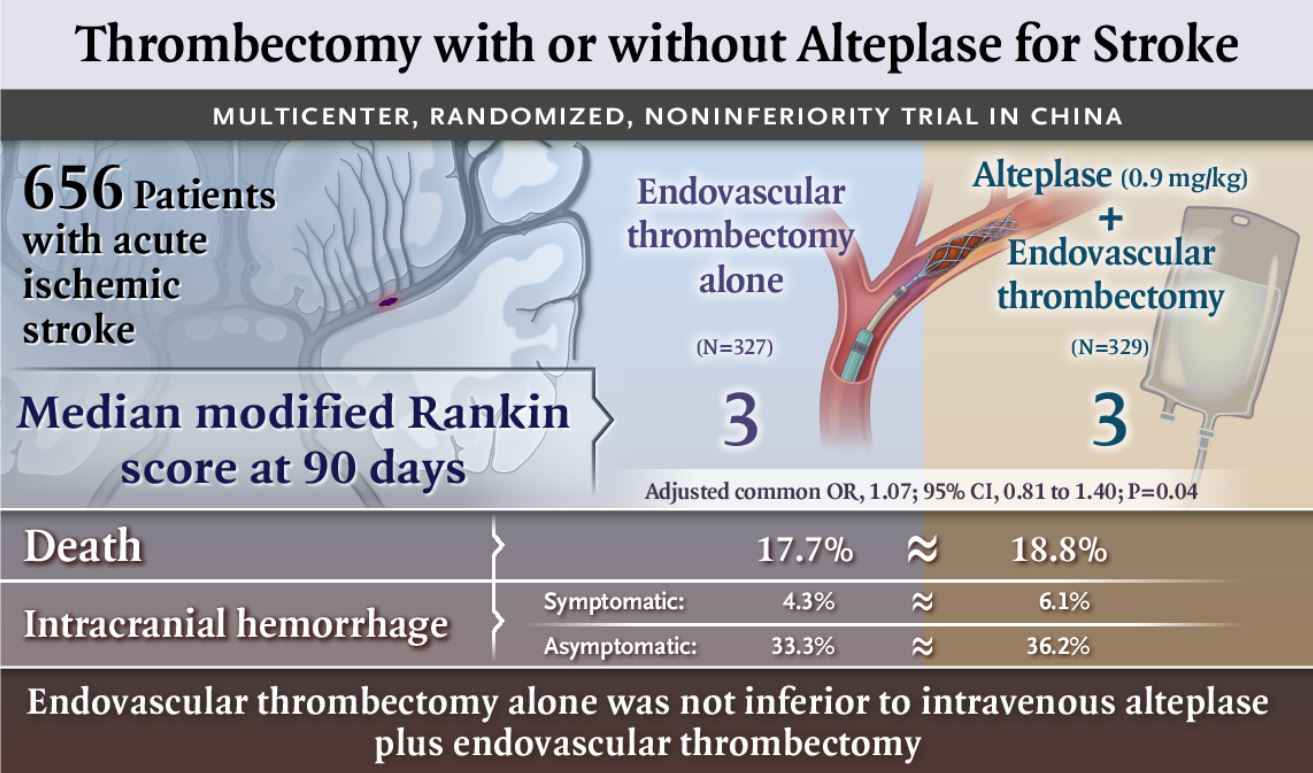
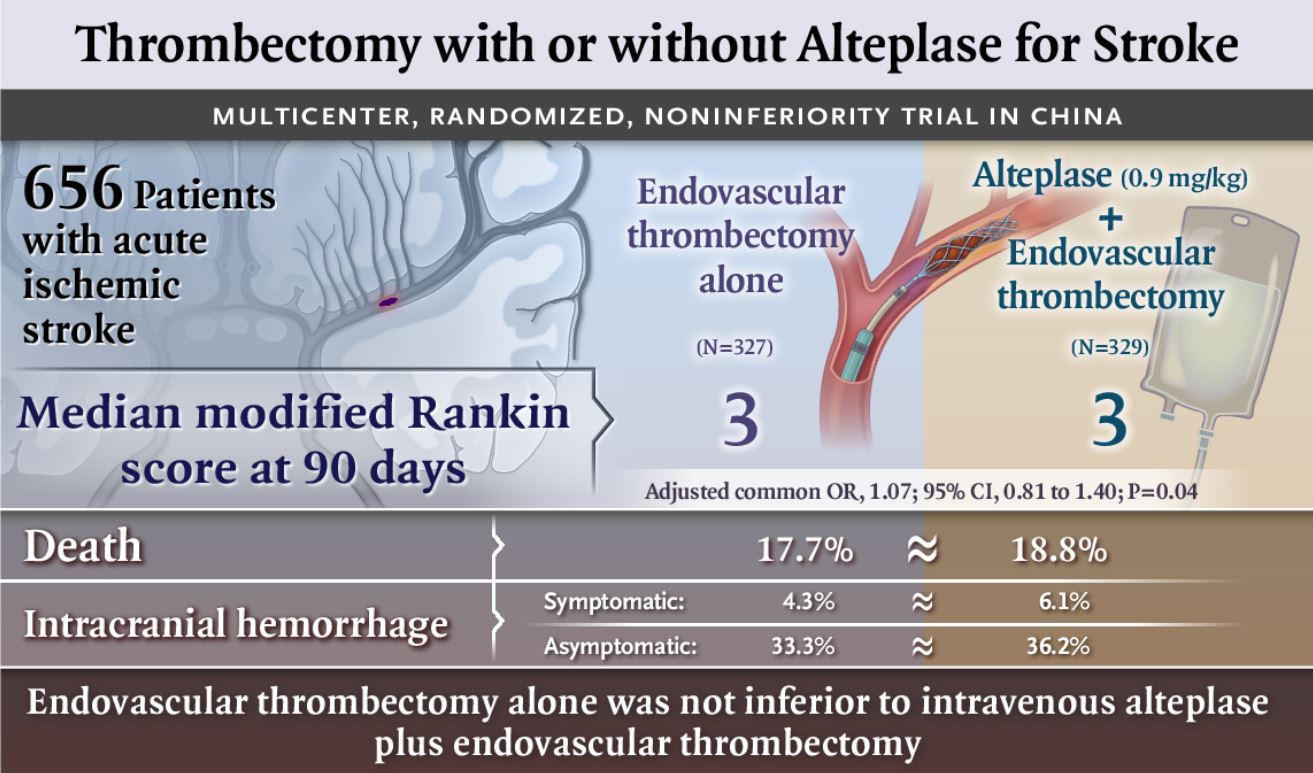
直接血管内治疗(DEVT)试验是一项比较发病4.5小时内,单独血管内治疗与阿替普酶静脉溶栓桥接血管内治疗急性大血管闭塞患者有效性及安全性的多中心、随机对照临床试验。该试验由陆军军医大学第二附属医院(重庆市新桥医院)神经内科主任杨清武教授科研团队联合全国32家医院协同开展,旨在优化急性前循环大血管闭塞患者救治方案的一项多中心随机对照临床试验。
1月19日,DEVT研究发表在世界四大顶级医学期刊之一JAMA《美国医学会杂志》上的结果显示,直接取栓并非劣于静脉溶栓桥接血管内治疗。下面,我们就来介绍一下该试验的具体发现。
该研究的目的只在探讨在大血管闭塞性卒中患者中,单用血管内溶栓术是否比静脉溶栓后再行血管内溶栓术在90天内达到功能独立的非劣势效果。为此,在中国33个卒中中心纳入了18岁以上、近端前循环颅内闭塞性卒中且症状发生后4.5小时内、符合静脉溶栓治疗条件的患者(n = 234)。入组时间为2018年5月20日至2020年5月2日,入组后进行为期90天的随访。
分别将上述患者随机分为单独的血管内血栓切除术组(n=116)和静脉溶栓桥接血管内血栓切除术组(n=118)。主要的随访终点事件是90天时达到功能独立的患者比例(定义为mRS 0-2分)。非劣势幅度为-10%。安全性结果主要包括48小时内有症状的脑内出血发生率和90天死亡率。
结果显示,在90天的随访中,单独的血管内血栓切除术组与桥接治疗组分别有63例(54.3%)与55例(46.6%)患者在90天的随访中实现了神经功能独立,非劣效性有意义(非劣效性P=0.003)。同样,两组的症状性脑内出血(6.1% vs 6.8%)和90天死亡率(17.2% vs 17.8%)也未发现组间显著差异。
研究人员由此认为,在发病4.5小时内的近端前循环闭塞导致的缺血性卒中患者中,与静脉注射阿替普酶加血管内治疗相比,单独的血管内治疗或静脉注射阿替普酶加血管内治疗相比,90天功能独立这一结果达到了预先规定的非劣效性统计阈值。这一结果也与去年发表在NEJM上的结论一致。
综上,本研究结果有力支持在有条件直接取栓的医院,跨过静脉溶栓,进行直接动脉取栓治疗,为急性卒中救治提供新策略,为卒中管理指南更新提供新证据,为减少个人和医保费用支出,减少家庭和社会经济负担提供新方法。
参考文献:
Zi W,et al. Effect of Endovascular Treatment Alone vs Intravenous Alteplase Plus Endovascular Treatment on Functional Independence in Patients With Acute Ischemic Stroke: The DEVT Randomized Clinical Trial. JAMA. 2021 Jan 19;325(3):234-243. doi: 10.1001/jama.2020.23523.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了
77
#Dev#
48
看到国内有设计不错的研究发表在顶级期刊,欣慰!
199
#EVT#
43
#取栓#
51
直接取栓并非劣于#静脉溶栓#桥接#血管内治疗#,这篇文章能入选2021年#十大#医学进展
664
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
131
涨知识
170
学习了
145
学习了,涨知识了!
107