ASCO2021:免疫表达信号可预测转移性结直肠癌的治疗反应和生存
2021-06-08 MedSci原创 MedSci原创
根据在2021年ASCO年会上提出的CALGB/SWOG 80405试验(摘要3515)的分析,肿瘤免疫信号影响转移性结直肠癌(mCRC)患者对治疗和生存的反应。

根据在2021年ASCO年会上提出的CALGB/SWOG 80405试验(摘要3515)的分析,肿瘤免疫信号影响转移性结直肠癌(mCRC)患者对治疗和生存的反应。
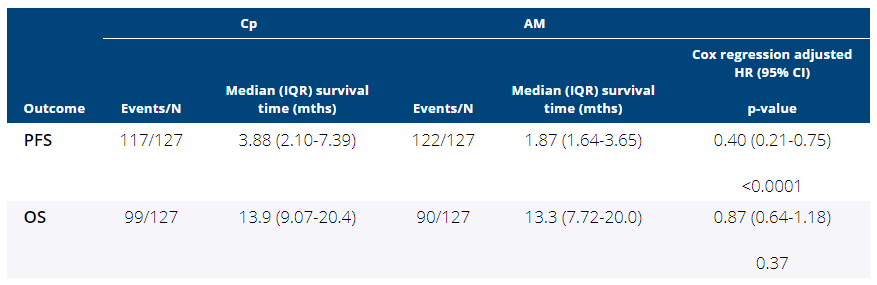
该随机III期试验比较了贝伐单抗联合化疗、西妥昔单抗联合化疗以及两种药物联合化疗在一线的情况;在总生存期(OS)方面没有发现差异。在这项新的分析中,由北卡罗来纳大学教堂山分校的医学博士Federico Innocenti领导的研究人员使用RNAseq分析了578例原发性肿瘤。他们发现了一些与较短OS相关的免疫信号。这包括M2巨噬细胞(HR 6.81, 95% CI[3.56, 30.16])和TGF-β (HR 1.37, 95% CI[1.03, 2.10])的信号表达增加。相反,浆细胞信号表达的增加与较长的OS相关(HR 0.52, 95% CI[0.27, 0.83])。记忆激活的CD4+ T细胞同样如此(HR 0.34, 95% CI[0.10, 0.66])。
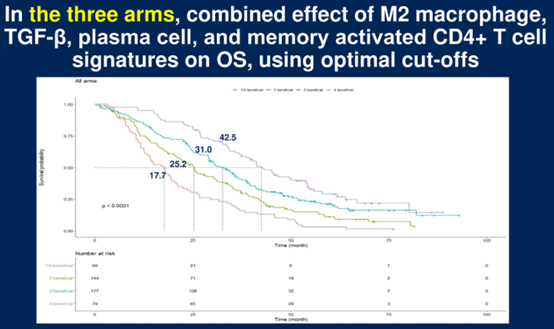
在所有研究中,当有益信号减少时,OS显著降低。当存在4个这样的信号时,中位OS为42.5个月;三个信号时为31.0个月,两个信号时为25.2个月,一个或零个有益信号时为17.7个月,且趋势非常显著。
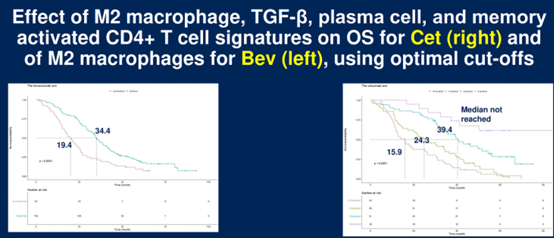
在贝伐单抗组中,只有M2巨噬细胞的信号表达增加与较短的OS相关(HR 6.64, 95% CI[2.74, 67.14]),而其他信号与生存差异无关。在西妥昔单抗组中,M2巨噬细胞的信号增加也同样如此(HR 4.31, 95% CI[2.12, 79.83]),但TGF-β也同样如此(HR 1.61, 95% CI[1.08, 4.04])。同样,在西妥昔单抗组中,浆细胞(HR 0.36, 95% CI[0.06, 0.55])和记忆激活的CD4+ T细胞(HR 0.37, 95% CI[0.03, 0.98])的信号增强与更长的OS相关。
在西妥昔单抗组中,有4个有益信号的患者中位OS未达到,其中有3个这样的信号的患者中位OS为39.4个月,有2个信号的患者中位OS为24.3个月,有1个或0个信号的患者中位OS为15.9个月。
在贝伐单抗组中,只有M2巨噬细胞信号与OS显著相关,存在有益信号的中位OS为34.4个月,无有益信号的中位OS为19.4个月。
Innocenti博士说,这些结果为治疗选择和开发新的活性组合(包括免疫检查点抑制剂)提供了新的标记物。Cleary博士对此表示赞同,并表示,这项试验以及今年在ASCO年会上提交的其他研究和其他最近的研究表明,RNA表达谱分析和其他分子技术在未来可能有助于识别患者进行靶向和免疫治疗。
然而,Cleary博士认为这些生物标记物需要进一步研究验证,这项研究表明,临床试验中仔细收集样本对于增进对这些疗法和其他疗法的了解至关重要。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ASC#
39
#转移性#
23
#结直肠#
39
很不错
85