陶凌:高危糖尿病合并冠心病患者的血脂管理
2020-12-31 《门诊》杂志 门诊新视野
众多循证证据表明,合并糖尿病的动脉粥样硬化性心血管疾病(ASCVD)患者不良事件风险显著增加。而进一步分析发现,这部分人群的血脂达标率明显偏低。
众多循证证据表明,合并糖尿病的动脉粥样硬化性心血管疾病(ASCVD)患者不良事件风险显著增加。而进一步分析发现,这部分人群的血脂达标率明显偏低,DYSIS-China研究显示,冠心病合并糖尿病患者的LDL-C达标率仅为39.7%。血脂达标是降低心血管事件风险的关键举措之一,重视对这部分人群的血脂管理势在必行。
糖尿病相关心血管事件 风险增加促进指南变迁
合并糖尿病的ASCVD患者心血管事件风险可显著增加。作为大型调脂治疗的研究FOURIER研究,在其亚组分析中,27,564例ASCVD患者随机接受依洛尤单抗或安慰剂治疗,11,031例患有糖尿病,16,533例无糖尿病(其中10,344例为糖尿病前期,6,189例血糖正常),随访2.2年。结果显示,在调整基线差异后,与无糖尿病ASCVD患者相比,合并糖尿病的ASCVD患者的主要终点事件风险比(HR)为1.26(P<0.0001),关键次要终点事件HR为1.40(P<0.0001)。
相类似的是,合并糖尿病的ACS患者早期死亡风险和MACCE发生率更高。根据CCC-ACS项目数据,研究纳入2014年11月至2017年6月期间,150家医院登记的63,450例ACS患者,评估中国ACS患者合并糖尿病是否与早期死亡风险和MACCE显著相关。研究表明,与非糖尿病ACS患者相比,合并糖尿病的ACS患者的全因死亡风险和MACCE发生率分别增加2倍和1.5倍。
基于此,《中国胆固醇教育计划调脂治疗降低心血管事件专家建议(2019)》提出,合并糖尿病的ASCVD患者为超高危患者,并将该部分患者的LDL-C目标值定为:<1.4 mmol/L(55 mg/dl)或较基线水平降低幅度≥50%;《超高危ASCVD患者血脂管理中国专家共识(2020)》提出,糖尿病是超高危ASCVD的高风险因素之一(超高危ASCVD定义:发生过1次严重的ASCVD事件合并≥2个高风险因素,或发生过≥2次严重的ASCVD事件),并将超高危ASCVD患者的LDL-C目标值定为:<1.4 mmol/L且较基线降幅≥50%(基线是指未接受降脂药物治疗时的LDL-C水平),而对于2年内发生≥2次MACE的患者,可考虑LDL-C降至1.0 mmol/L以下且较基线降幅超过50%以上;2019 ESC/EAS指南提出,糖尿病伴有靶器官损伤(微量蛋白尿,视网膜病变或肾病)或至少3个主要危险因素,或早发1型糖尿病>20年为心血管疾病极高危人群,并对这部分人群的LDL-C目标值进行了明确。(表1)
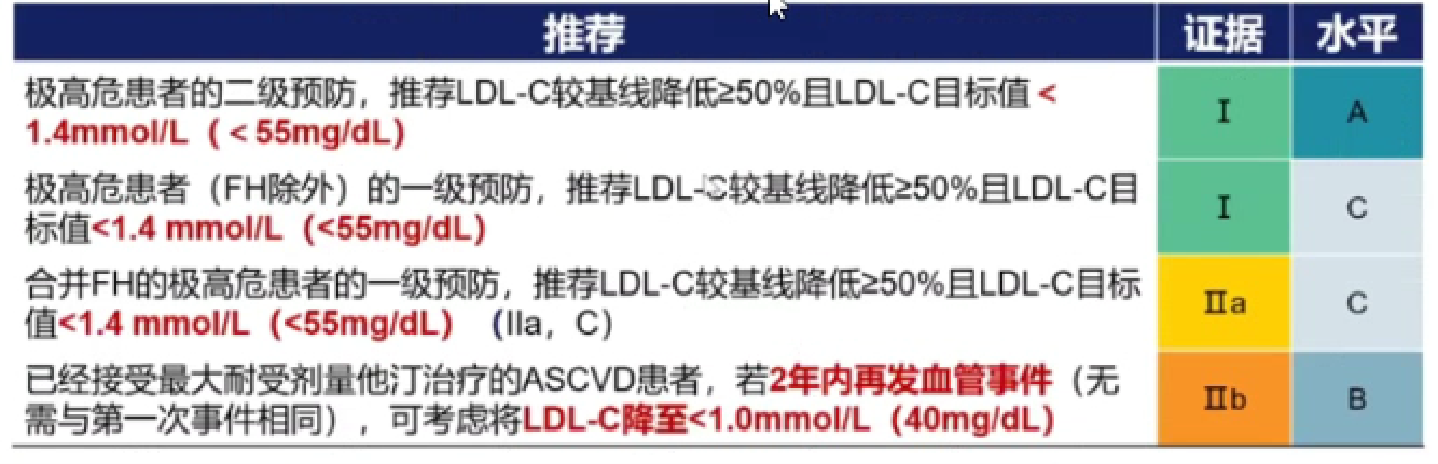
表1. 2019 ESC/EAS指南对于极高危患者的LDL-C目标值推荐
新型调脂药物异军突起
上述介绍了糖尿病患者降脂相关指南推荐,而在现实临床中,糖尿病患者的血脂控制现状不容乐观。DYSIS研究糖尿病亚组分析结果显示,尽管将LDL-C目标值定为2.5 mmol/L,仍有将近40%的冠心病合并糖尿病的患者经过治疗,LDL-C仍未达标;DYSIS-China研究提示,冠心病合并糖尿病患者的LDL-C达标率仅为39.7%。因此,强化糖尿病合并心血管疾病患者的降脂治疗势在必行。
虽然他汀是降脂治疗的基石,但由于其本身存在的“6规则”,即他汀剂量增倍仅带来额外6%的LDL-C水平降低,故他汀单药治疗LDL-C降幅有限;且大剂量他汀单药治疗可能增加12%的新发糖尿病风险;再加上大剂量他汀单药治疗不良事件发生风险高于中等剂量他汀治疗。因此,他汀在进一步强化降脂治疗方面效果有限。
新型调脂药物依折麦布和PCSK9抑制剂的出现为临床医师进行强化降脂治疗提供了有利的武器。在机制上,他汀通过抑制肝脏胆固醇的合成、依折麦布通过抑制肠道胆固醇的吸收、PCSK9抑制剂通过使肝脏表达更多的LDL-R进而降低血浆LDL-C水平。因此,三种药物在降脂方面具有机制互补的效果。
临床中,这两种新型降脂药物的确可给糖尿病患者带来更多获益。以依折麦布为例,IN-CROSS研究事后分析结果显示,经6周治疗,依折麦布/辛伐他汀(10/20 mg,n=313)联合治疗的心血管疾病高危T2DM患者,LDL-C降幅显著优于瑞舒伐他汀患者(-30.3% vs. -11.5%),进而使得依折麦布/辛伐他汀组的LDL-C达标率明显高于瑞舒伐他汀组。(图1)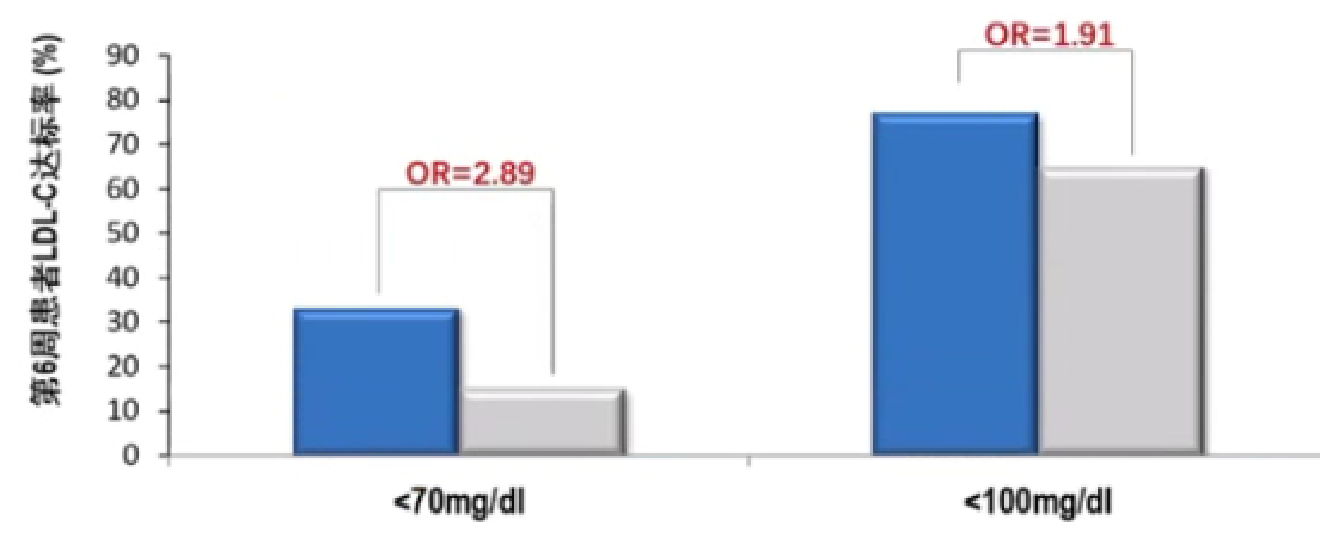
图1. 心血管疾病高危的T2DM患者采用依折麦布与他汀联合LDL-C达标率更高
荟萃分析也显示,依折麦布联合他汀可显著降低T2DM患者LDL-C。一项纳入27项随机、双盲、对照研究的汇总分析结果显示,对于T2DM患者,接受依折麦布/他汀治疗的患者LDL-C降幅明显高于接受他汀单药治疗的患者(-41.1% vs. -23.7%)。
同样,PCSK9抑制剂也在糖尿病患者的调脂治疗方面发挥了重要作用。上述提到的FOURIER亚组分析结果表明,在合并糖尿病的ASCVD患者中,依洛尤单抗治疗可使主要终点事件相对风险降低17%,绝对风险降低2.7%;而在未合并糖尿病的ASCVD患者中也看到了相似的结果。此外,在该研究的关键次要终点事件方面也显示出类似的结果。(图2)
图2. FOURIER亚组:依洛尤单抗治疗可给ASCVD合并糖尿病患者带来显著主要终点事件获益
循证加速调脂策略转变
基于此,《中国胆固醇教育计划调脂治疗降低心血管事件专家建议(2019)》提出:
(1)对于极高危患者(糖尿病合并高血压或糖尿病合并1项其他危险因素且LDL-C≥3.4 mmol/L)
要求LDL-C<1.8 mmol/L(70 mg/dl),可在生活方式改变的基础上启动他汀类药物治疗;
如他汀类药物治疗后LDL-C仍≥1.8 mmol/L(70 mg/dl),建议联用依折麦布,如仍不达标,可考虑加用PCSK9抑制剂;
对于采用联合治疗仍不能达标的患者,要求LDL-C较基线值降≥50%。
(2)对于超高危患者(ASCVD合并糖尿病)
要求LDL-C<1.4 mmol/L(55 mg/dl),可在生活方式改变的基础上启动他汀类药物治疗,对于LDL-C基线值较高的患者可直接启动他汀类药物与依折麦布联合治疗;
如使用他汀类药物联合依折麦布治疗LDL-C仍≥1.4 mmol/L(55 mg/dl),建议加用PCSK9抑制剂;
如预估他汀类药物加用依折麦布不能使患者LDL-C达标,也可直接启动他汀类药物与PCSK9抑制剂联合治疗;
对于采用联合治疗仍不能达标的患者要求LDL-C较基线值降低≥50%。
另外,《超高危ASCVD患者血脂管理中国专家共识(2020)》也给出了更为细致的超高危ASCVD患者的调脂策略。(图3)

图3. 《超高危ASCVD患者血脂管理中国专家共识(2020)》调脂策略建议
此外,2019欧洲血脂指南也建议:
如使用最大可耐受剂量的他汀类药物后无法达到降脂目标,建议联合使用依折麦布(I,B);
对于极高危患者的二级预防,如使用最大耐受剂量他汀类药物和依折麦布后仍未能达到目标血脂水平,建议联合使用PCSK9抑制剂(I,A);
如最大耐受剂量他汀类药物和依折麦布治疗4~6周LDL-C仍未达标,可联用PCSK9抑制剂(I,B)。
而在甘油三酯(TG)的管理方面,《中国T2DM合并血脂异常防治专家共识(2017年修订版)》提出:如患者TG>5.6 mmol/L时,可在生活方式干预的基础上首选降TG药物治疗(如贝特类,或高纯度鱼油),以减少发生急性胰腺炎的风险(推荐;C级证据);经过中等强度的他汀类药物治疗后non-HDL-C仍不达标者,特别是TG≥2.3 mmol/L,可在他汀类药物治疗基础上加用贝特类药物(建议;B级证据)。
值得注意的是,在糖尿病患者的常用药物中,部分药物可对患者的血脂产生一定影响。(图4)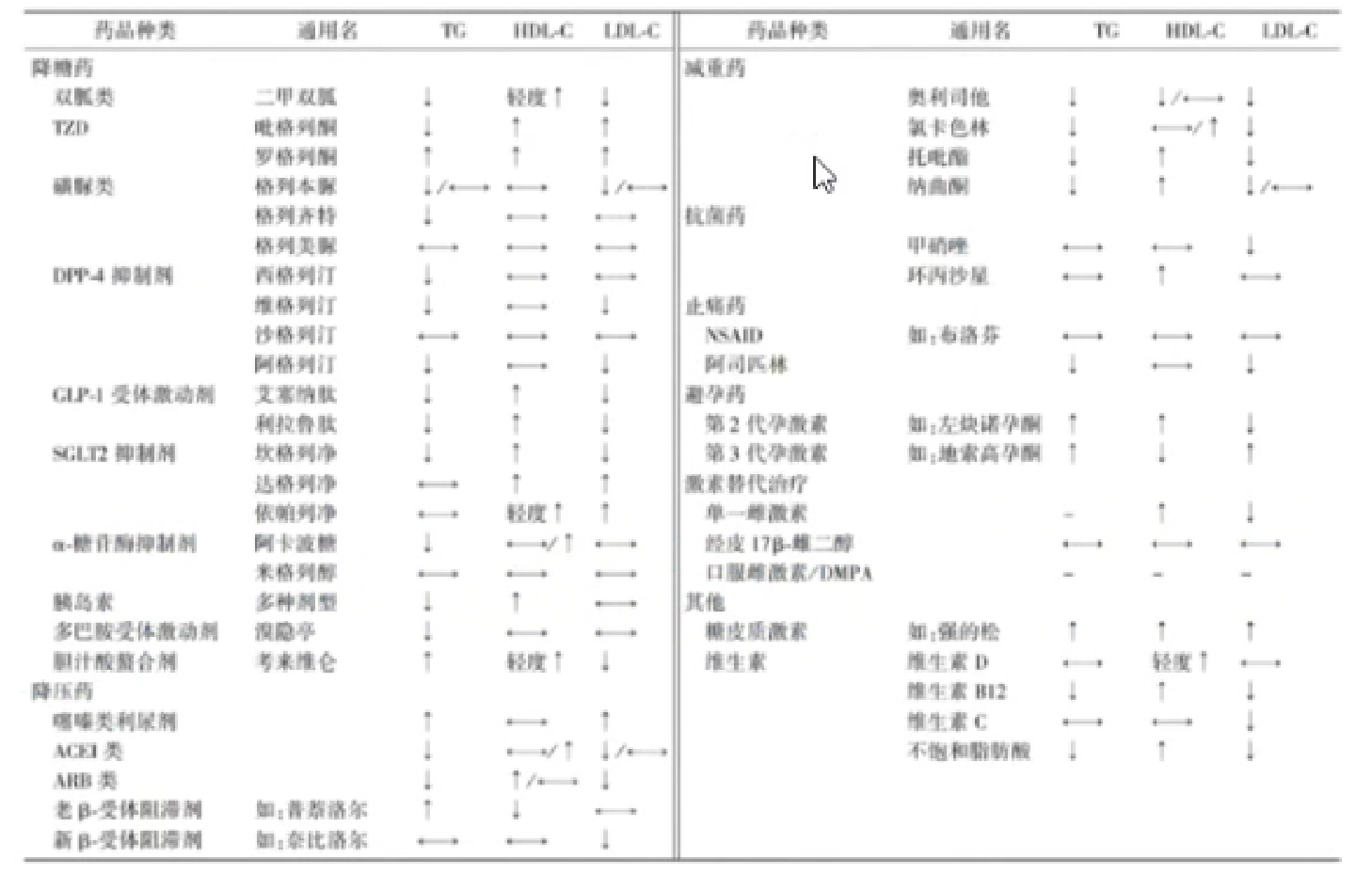
图4. T2DM患者常用药物对血脂的影响
总 结
合并糖尿病的ASCVD患者不良事件风险显著增加,而该部分人群的血脂达标率明显偏低。他汀单药治疗因降幅受限、副作用增加等因素,联合应用新型调脂药物依折麦布和PCSK9抑制剂是合并糖尿病ASCVD患者血脂达标的有力武器,近年来得到了各国指南的广为推荐。相信新型调脂药物必将为合并糖尿病的心血管疾病患者带来更多获益。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了
75
学习了
97
#冠心病患者#
54
谢谢MedSci提供最新的资讯
58
学习了
96
众多循证证据表明,合并糖尿病的动脉粥样硬化性心血管疾病(ASCVD)患者不良事件风险显著增加。
93