本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
2021-11-21 吴汉平 胃肠病
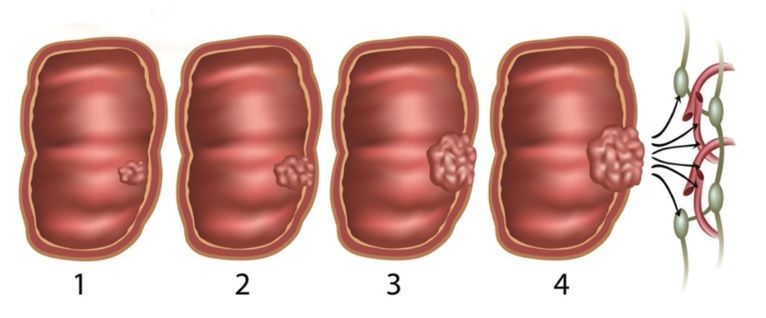
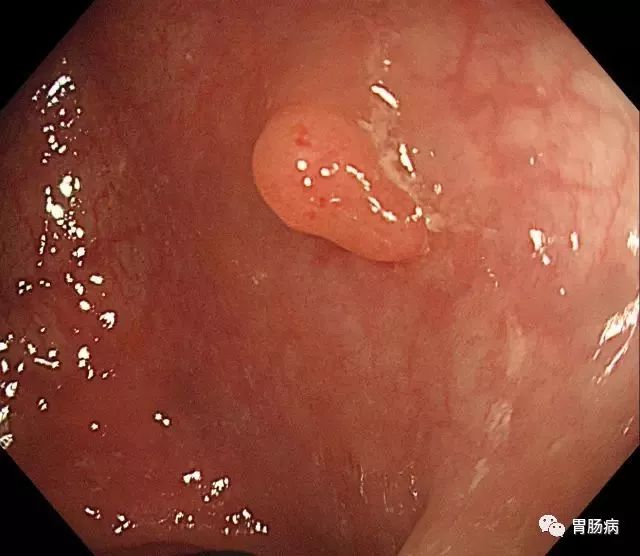
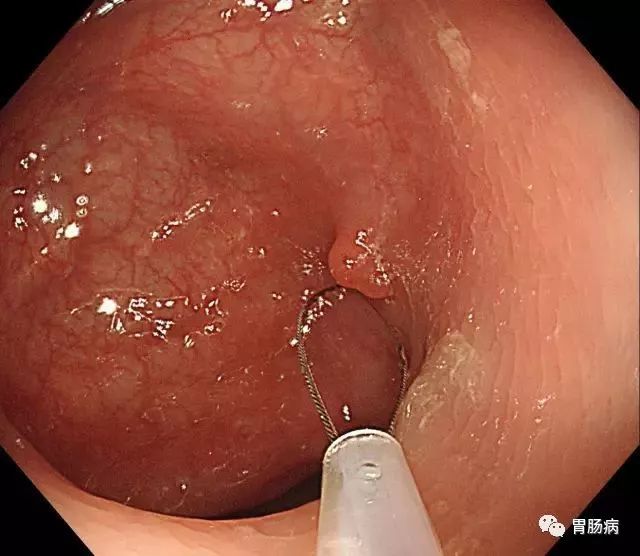
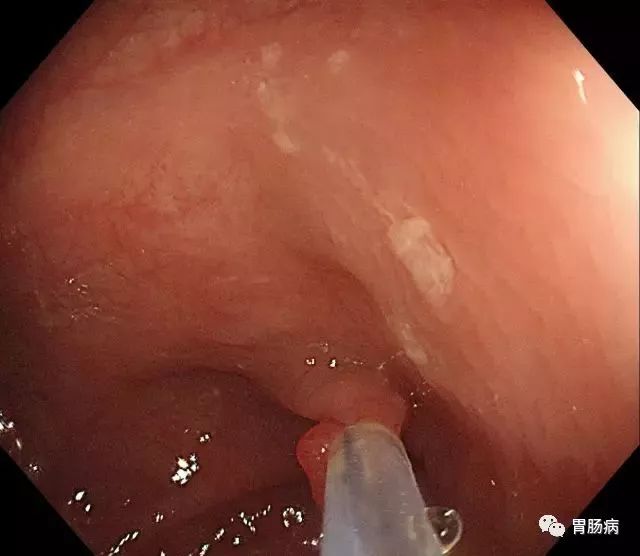
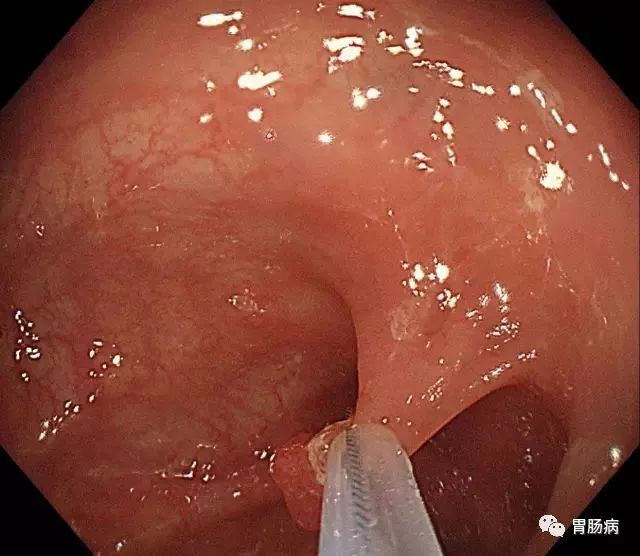
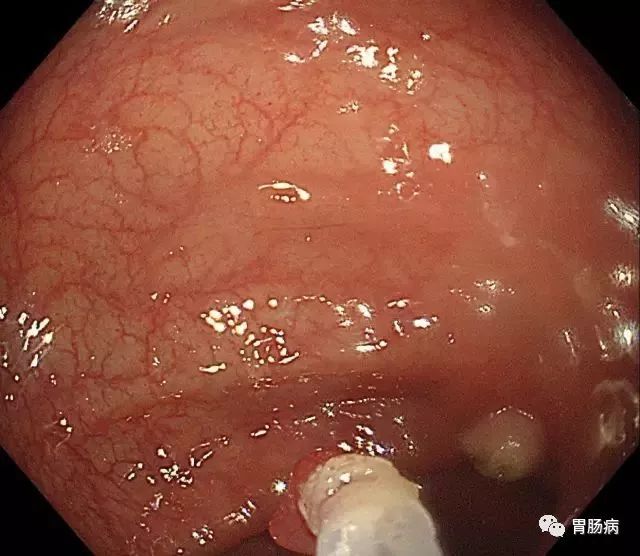
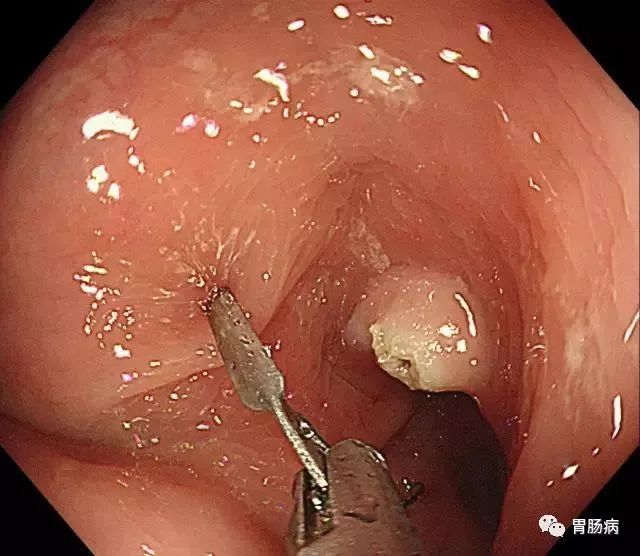
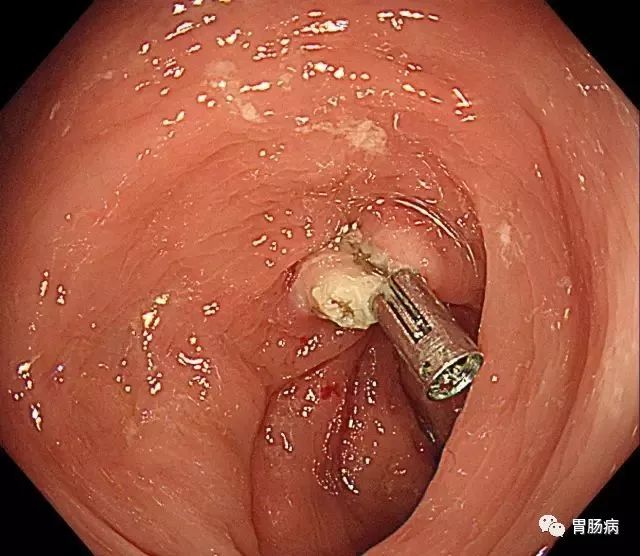
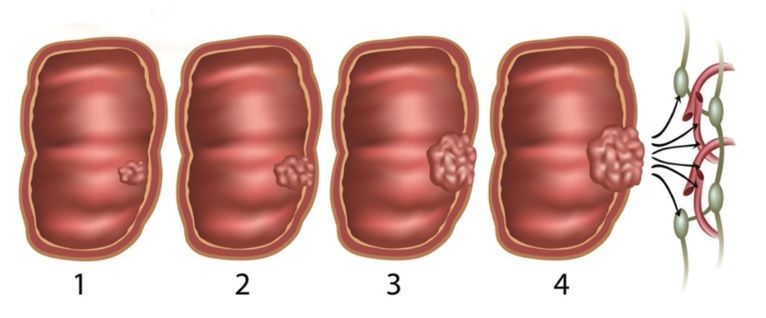
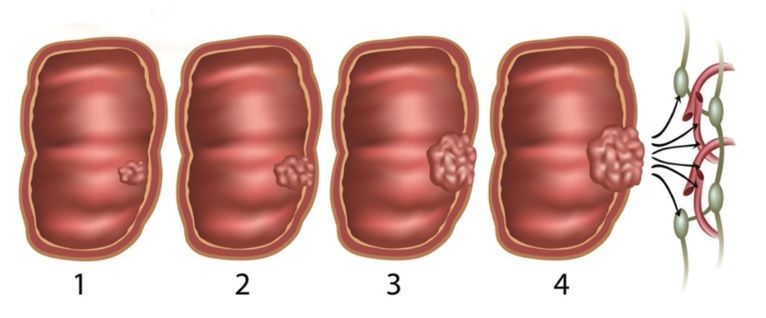
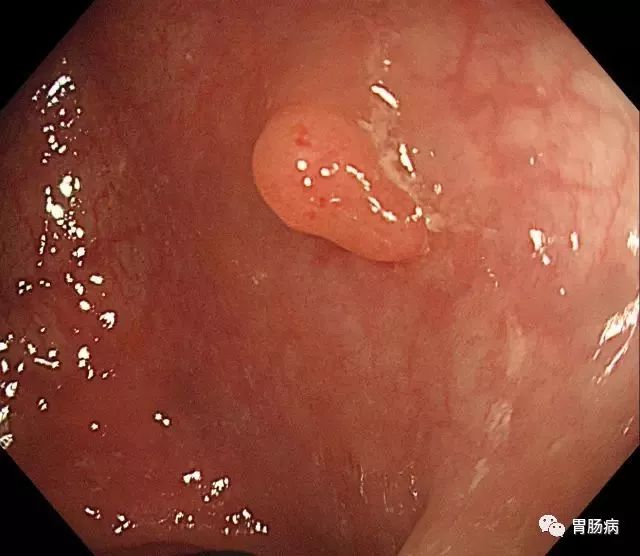
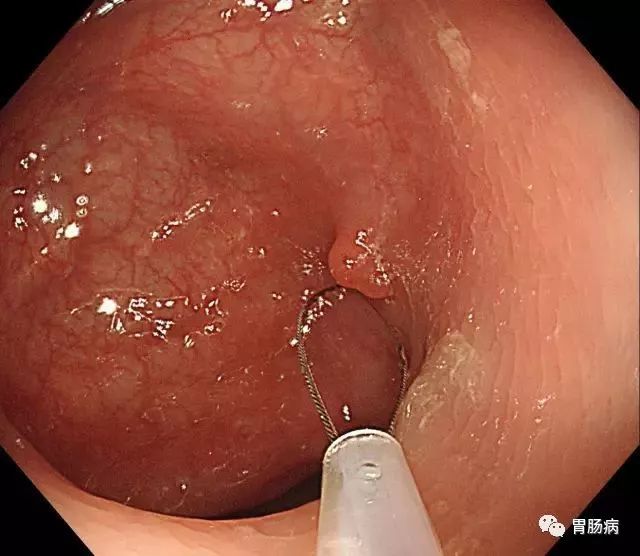
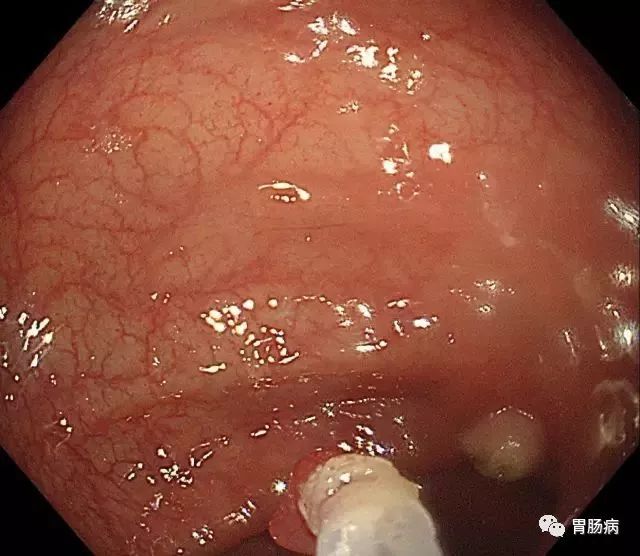
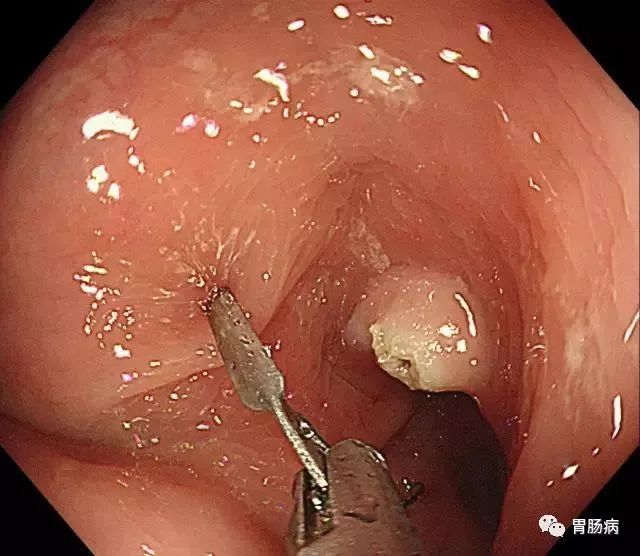
大肠息肉术后容易复发,所以应定期行肠镜+病理复查。复查的频率应当根据具体情况而定。

对于医生来说,放屁虽然会让人陷入尴尬,但是不放屁可就未必是一件好事了,它往往意味着身体出现了一些问题。
近日,娱乐圈经纪人杨天真晒出一段视频,称自己要去做切胃手术。杨天真透露,朋友听到她要做切胃手术后都纷纷来劝阻她,希望她能通过控制饮食或者运动来减肥瘦身。
收藏学习!
随着社会老龄化进程加速,骨质疏松症的患病率迅猛增加,肌少症如影随行,共同引发多重并发症,导致老年人群生活质量下降,并给社会带来沉重经济负担。


梅斯医学MedSci APP
医路相伴,成就大医
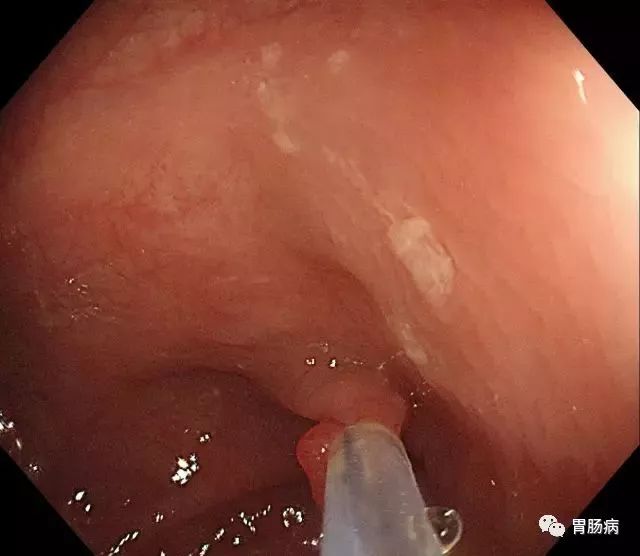
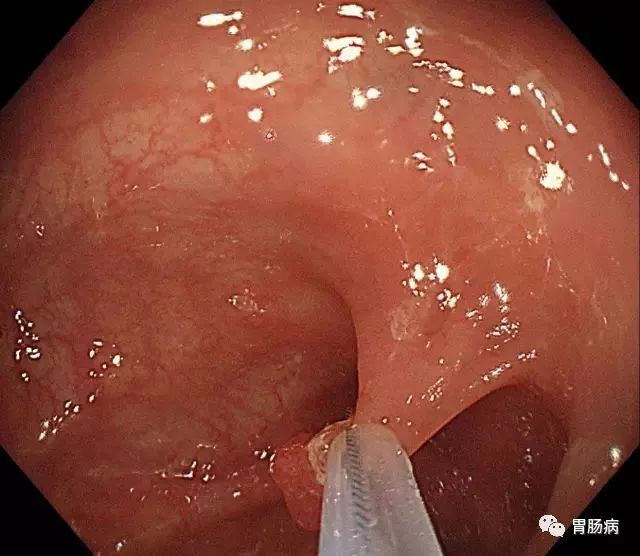
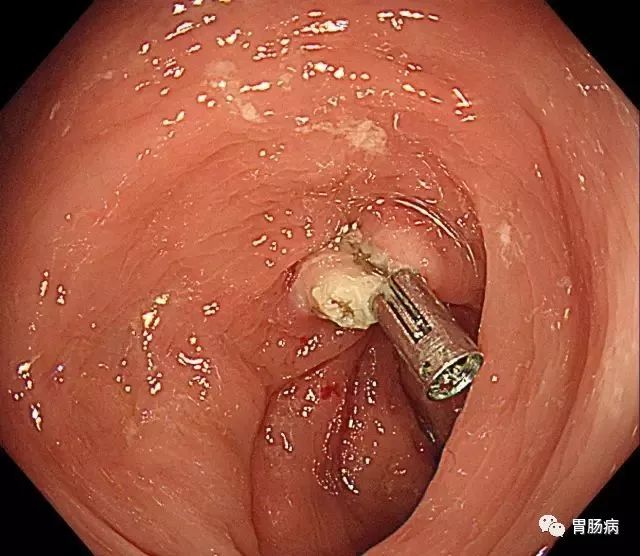
#切除术#
32
受益匪浅
39
中位随访时间分别为10.7个月(范围= 0.2
60
学习了
67