IBD: 心理承受能力与IBD患者的更少疾病活动,更好的生活质量以及更少的炎症性肠病手术相关
2021-05-21 MedSci原创 MedSci原创
炎症性肠病(IBD)包括溃疡性结肠炎(UC)和克罗恩病(CD)两种疾病,在美国影响超过了100万人口,在欧洲影响250万了人口。
炎症性肠病(IBD)包括溃疡性结肠炎(UC)和克罗恩病(CD)两种疾病,在美国影响超过了100万人口,在欧洲影响250万了人口。这些疾病有可能极大地影响一个人的生活历程和个人选择,而较高的心理适应能力可以促进IBD的良好预后。但是一旦心理承受能力不佳则造成了巨大的心理负担,可能会导致肠损伤,疲劳和残疾,从而给患者带来持续的压力。一个人从逆境中恢复的能力是否会影响疾病进程尚不清楚。这项研究的目的是探究韧性和IBD疾病活动性,生活质量(QoL)和IBD相关手术之间的关系。

研究人员在一个医疗中心招募了符合条件的IBD患者,所有患者均按要求填写了Connor-Davidson弹性量表问卷,该问卷用于测量心理承受能力(高弹性评分≥35)。主要结局是IBD疾病活动度,通过Mayo评分和Harvey-Bradshaw指数(HBI)分别对UC和CD进行评估,同时研究人员还评估了QoL和IBD相关的手术情况。进行了多元线性回归,以评估高适应力与疾病活动性和生活质量的关系。

本项研究共包括了92例溃疡性结肠炎(UC)和137例克罗恩病(CD)患者。在27%的UC患者和21.5%的CD患者中发现患者的心理承受能力较高。在UC患者中,高弹性心理承受能力的患者的平均Mayo得分为1.54,低弹性患者的平均Mayo得分为4.31,P <0.001。在CD患者中,高弹性患者的平均HBI为2.31,低弹性患者的平均HBI为3.95,P = 0.035。在多变量分析中,高心理承受能力与UC(P <0.001)和CD(P = 0.037)的QoL改善有关。同时高心理承受能力还与CD患者中较少的手术相关(P = 0.001)。
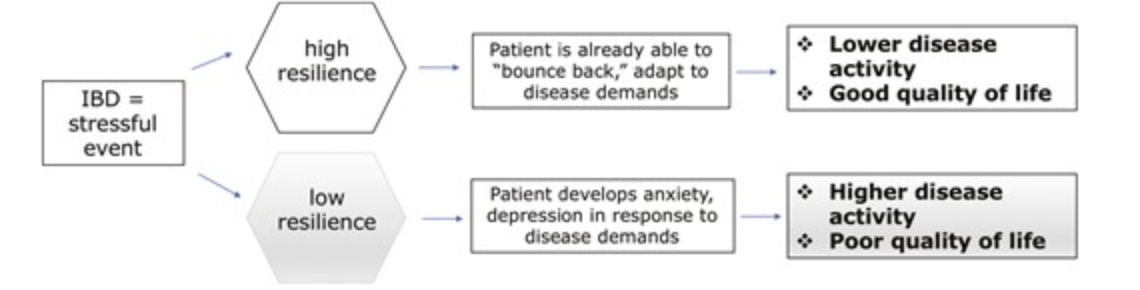
本项研究证实高心理承受能力与IBD患者疾病活动度降低和QoL改善以及CD患者手术次数减少独立相关。
原始出处:
Priya Sehgal. Et al. High Levels of Psychological Resilience Associated With Less Disease Activity, Better Quality of Life, and Fewer Surgeries in Inflammatory Bowel Disease. Inflammatory Bowel Diseases.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#疾病活动#
43
#IBD#
25
#炎症性#
27
赞
69