Nature Medicine:重磅!晚期癌症患者100%治疗反应!88%完全缓解!双特异性靶点CAR-T疗法1期临床试验结果公布
2021-07-30 “上海细胞治疗工程技术研究中心”公众号 “上海细胞治疗工程技术研究中心”公众号
再给CAR-T细胞一个识别的靶点,双倍识别,可以更好地发挥治疗效果.
关于CAR-T细胞疗法在血液肿瘤中的强大治疗效果,在之前的多篇文章中我们都已经做过介绍。但是在接受CAR-T细胞治疗后,有一部分患者会面临再次复发的情况。在对这些患者进行复查后发现很多患者会丢失掉CAR-T细胞针对的靶点从而导致疗法失效。
举个例子,目前CAR-T细胞疗法最常见的治疗靶点就是CD19,——这个CD19就相当于是癌细胞的特征,只要是有这个靶点的癌细胞都会被找到并且被消灭。狡猾的癌细胞为了不被消灭,就想办法隐藏或者降低CD19的表达,这样失去了癌细胞的特征性靶点,CAR-T细胞自然无法针对性的进行杀伤。而针对CD19靶点的CAR-T细胞一般就被叫做CD19-CAR-T细胞。
T细胞(图片来源:Pixabay官网)
有没有什么办法可以解决这个问题呢?为此,研究人员想到:既然识别1个靶点失效了,那么我们再加一个识别靶点是不是可行呢?简单来说,就是再给CAR-T细胞一个识别的靶点,双倍识别,可以更好地发挥治疗效果——而另一个选择的靶点也是B细胞经常表达的一个分子CD22,从而构建了双特异性靶点CD22-CD19-CAR-T细胞疗。
那么双特异性靶点CAR-T细胞疗法的治疗效果如何呢?发表在《Nature Medicine》杂志上1期临床试验就公布了最新的治疗数据!
本次研究中,一共有39名患者被纳入研究,包括17名急性B细胞淋巴细胞白血病(B-ALL)患者和22名高危大B细胞淋巴瘤(LBCL)患者,最终有38名患者接受了CD22-CD19-CAR-T细胞疗法。
值得注意的是,在平均中位年龄为47岁的B-ALL患者群体中,有71%的患者是接受过同种异体造血细胞移植 (HCT) 后疾病进展,其中有65%此前接受过CD19定向治疗(包括1例患者此前接受过CAR-T细胞治疗),同时有29%的患者此前接受过CD22治疗。LBCL队列的患者此前均为接受过CAR-T细胞治疗,其中也有4名接受过自体干细胞移植。这些患者均是在多项治疗后疾病进展的情况下接受了双特异性靶点CAR-T细胞疗法。
首先,我们来看下B-ALL患者在接受治疗后的反应,主要反应评估在接受治疗后28天进行评估。结果如下:
所有的17例患者病情均达到缓解,整体缓解率100%;
其中14例患者完全缓解,完全缓解率82%:
剩下的3例患者为部分缓解。
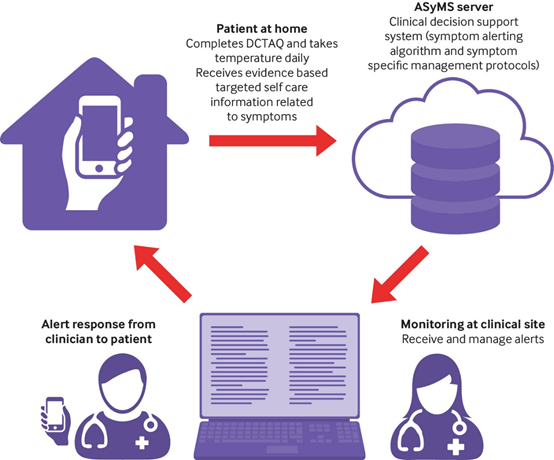
另外在此研究中有一名患者在接受治疗后6个月病情得到了改善,使得整体的完全缓解率上升达到了88%,患者的情况如下图所示:在接受治疗后6个月,发现整体情况出现了缓解。

1位患者在接受治疗后6个月出现缓解情况(图片来源:参考资料1)
B-ALL患者的中位随访时间为9.3个月,患者的中位总生存期为11.8个月,无进展生存期为5.8个月。
另一组LBCL患者主要反应评估则是在接受治疗3个月后进行。整个队列的总体反应率为62%,完全缓解率为29%,平均中位随访时间为10个月,中位总生存期为22.5个月,并且可能会随着随访时间的继续而延长。
另外研究人员对肿瘤样本可以评估的患者进行了ct DNA检测,其中在持续缓解的患者体内未检测到ct DNA,而临床进展的患者则出现了ct DNA升高的情况,这也表明ct DNA对于判断治疗后患者的反应有着对应的指导意义。

对LBCL患者进行的ct DNA检测
当然,作为双靶点的CAR-T细胞疗法,其治疗副作用是否更大呢?在本次治疗中,有29名患者出现细胞因子风暴(CRS),但多数级别较低,2名患者出现了3级及以上的CRS;其中14名出现了神经毒性反应,4人为3级及以上的神经毒性反应,出现的副作用都得到了有效应对和控制。
从本次的1期临床实验结果来看,双特异性靶点的治疗效果十分喜人。同时,CAR-T细胞疗法也有了很多创新的实验,比如利用CAR-T细胞在肿瘤部位释放PD-1抗体,在肿瘤局部解除免疫抑制,更好地发挥抗肿瘤作用。
原始出处:
Spiegel, J.Y., Patel, S., Muffly, L. et al. CAR T cells with dual targeting of CD19 and CD22 in adult patients with recurrent or refractory B cell malignancies: a phase 1 trial. Nat Med (2021). https://doi.org/10.1038/s41591-021-01436-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CAR-#
22
#DIC#
30
#结果公布#
47
#特异性#
33
#CIN#
27
#完全缓解#
25
#晚期癌症患者#
0
#Nat#
21
#癌症患者#
24
#重磅#
25