Nature:“坏胆固醇”原来是这样进入血管内壁的...
2019-04-26 不详 中国生物技术网
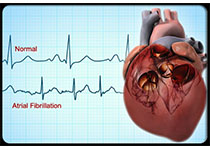
近日,美国德克萨斯大学西南医学中心(UTSW)的研究人员确定了体内循环的“坏胆固醇”如何进入动脉壁,并产生斑块使血管变窄,从而导致心脏病发作和中风。这项研究4月24日已发表在《Nature》上。研究通讯作者、肺与心血管生物学中心的负责人、儿科学教授Philip Shaul博士说,低密度脂蛋白(LDL)胆固醇进入动脉壁会导致动脉粥样硬化或动脉硬化的发展,而动脉粥样硬化会进一步导致心脏病发作和中风。因
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
40
学习了谢谢分享
74
优秀
85
学习,谢谢分享!
85
学习了谢谢分享
87