Circulation:葛均波,孙爱军团队发现预防和治疗主动脉夹层的新靶点
2022-04-30 MedSci原创 MedSci原创 发表于威斯康星
主动脉瘤和主动脉夹层(TAD)在全球的发生率为1.3%-8%,主动脉夹层破裂导致的死亡率约为90%。在国内每年新发病例20万,其中97.5%的病人因得不到及时有效治疗,或死亡或随时面临死亡,仅有2%的
主动脉瘤和主动脉夹层(TAD)在全球的发生率为1.3%-8%,主动脉夹层破裂导致的死亡率约为90%。在国内每年新发病例20万,其中97.5%的病人因得不到及时有效治疗,或死亡或随时面临死亡,仅有2%的患者获得手术机会幸存。主动脉夹层在中国每年带来的经济负担超过100亿元人民币。早期诊断对于提高主动脉夹层患者的生存率至关重要。临床上预防主动脉退行性变和减缓疾病进展的有效药物很少。因此,探讨夹层的发病机制和生物标记物,对于指导预防或者治疗主动脉夹层具有重要临床意义。
在国家自然科学基金项目等资助下,中国科学院院士、复旦大学附属中山医院心内科主任葛均波教授、孙爱军教授领衔的研究团队在平滑肌细胞表型转化调控主动脉夹层的研究中取得新进展,研究成果以“Legumain介导的平滑肌细胞表型转化促进主动脉夹层(Legumain Is an Endogenous Modulator of Integrin αvβ3 Triggering Vascular Degeneration, Dissection, and Rupture)”为题,于2022年1月31日发表在《循环》(Circulation)杂志(IF=30)上。文章第一作者为潘丽虹博士、柏佩原博士、翁鑫宇博士后、刘进硕士。复旦大学特聘教授胡凯教授在稿件修改过程作出了贡献。

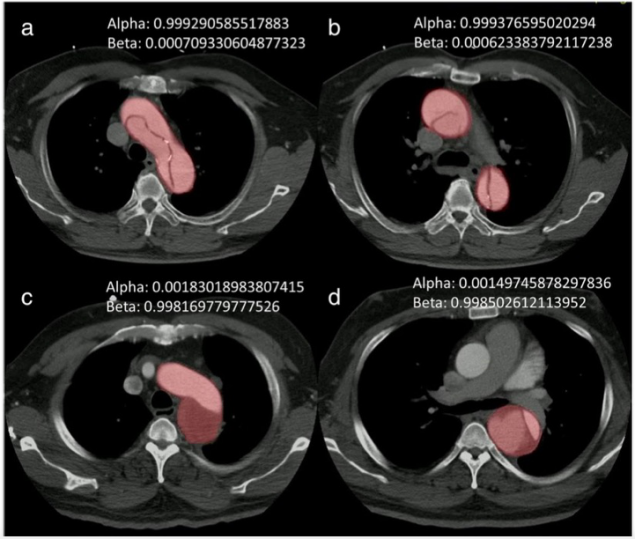
图.巨噬细胞分泌的Lgmn结合到平滑肌细胞表面的整合素αvβ3,并抑制GTP酶的活化,从而减少平滑肌细胞收缩型标志物的转录
Legumain(Lgmn)是一种溶酶体半胱氨酸蛋白酶,在动脉粥样硬化以及心肌梗死等心血管疾病中发挥重要作用。该研究从来自 GEO 数据库的微阵列数据表明,TAD 患者和 Ang II 诱导的腹主动脉瘤 (AAA) 小鼠的主动脉中 Lgmn 上调。TAD 患者和 BAPN 诱导的 TAD 小鼠的主动脉和血清中证实了 Lgmn 升高。在 Lgmn 缺陷或抑制的小鼠中,BAPN 诱导的 TAD 进展显著改善。Lgmn 的巨噬细胞特异性缺失减轻了 BAPN 诱导的 ECM 降解。同时Lgmn 巨噬细胞特异性缺失改善了 BAPN 治疗小鼠的 VSMC 表型转换。通过巨噬细胞和 VSMC 共培养系统评估,巨噬细胞衍生的 Lgmn 在体外抑制 VSMC 分化。机制上,巨噬细胞衍生的 Lgmn 与 VSMC 中的整合素 αvβ3 结合并阻断整合素 αvβ3,因此减弱 Rho GTPase 激活,下调 VSMC 分化标志物并最终加剧 TAD 发展。Rho 激酶 (ROCK) 抑制剂 Y-27632 逆转了 Lgmn 缺失在主动脉夹层中的保护作用。总之,该研究表明 Lgmn 信号可能是预防和治疗TAD的新靶点。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新靶点#
37
#主动脉#
42
#动脉夹层#
52
#主动脉夹层#
82
这个研究不错,厉害了!!!谢谢分享
85