Eur Urol Focus:Avelumab联合甲磺酸艾日布林治疗转移性尿路癌
2021-03-31 AlexYang MedSci原创
转移性尿道癌(mUC)患者预后较差,因此需要进一步开发针对这些患者的新型组合药物。
转移性尿道癌(mUC)患者预后较差,因此需要进一步开发针对这些患者的新型组合药物。

最近,有研究人员评估了艾日布林与avelumab联用的安全性和有效性。研究是一项开放标签的1b期研究,其中顺铂不符合、治疗无效或铂类耐药的mUC患者接受艾日布林和avelumab治疗。研究人员采用了3+3设计。由于免费研究药物无法获得,研究提前终止,但研究人员对纳入研究的患者进行了延长随访。
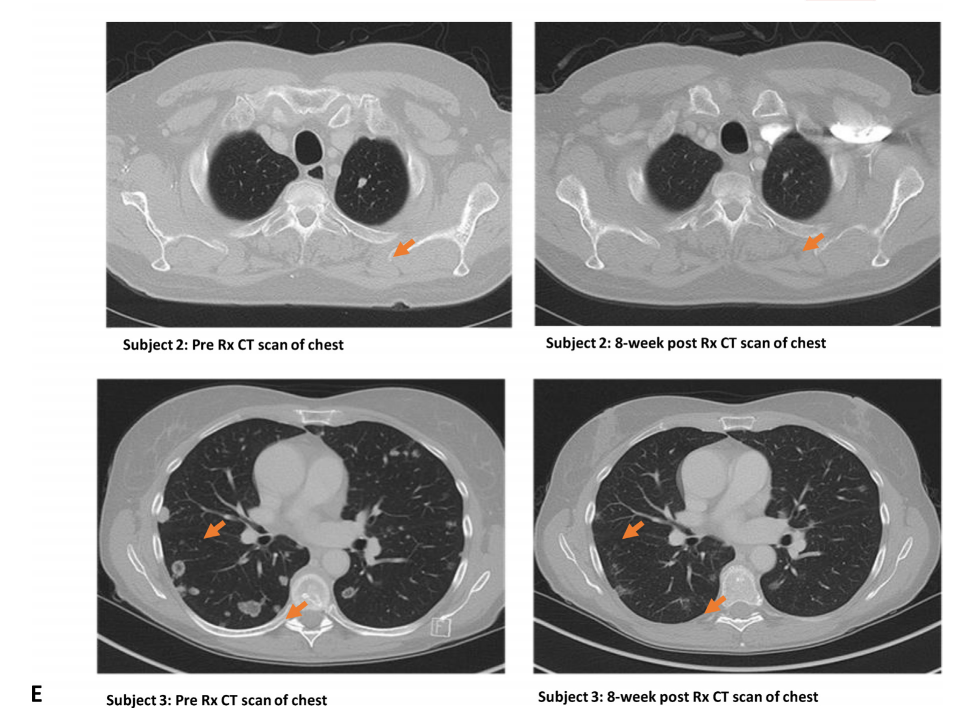
MTD组共有6名患者入组(0队列中n=3名,+1队列中n=3名)。0组患者在每28天的第1天和第15天接受艾日布林1.1 mg/m2 + avelumab 10mg /kg治疗,+1组患者在每28天的第1天和第15天接受艾日布林1.4 mg/m2 + avelumab 10mg /kg治疗。研究发现,在队列0中没有观察到剂量限制性毒性(DLT),而在队列+1中观察到两个DLT事件。在队列0中,有2名患者的部分反应是持久的,其中1名患者有7.8个月的持久反应。 在4/6名患者中观察到疾病控制(66.7%)。由于提前终止,无法确定MTD。
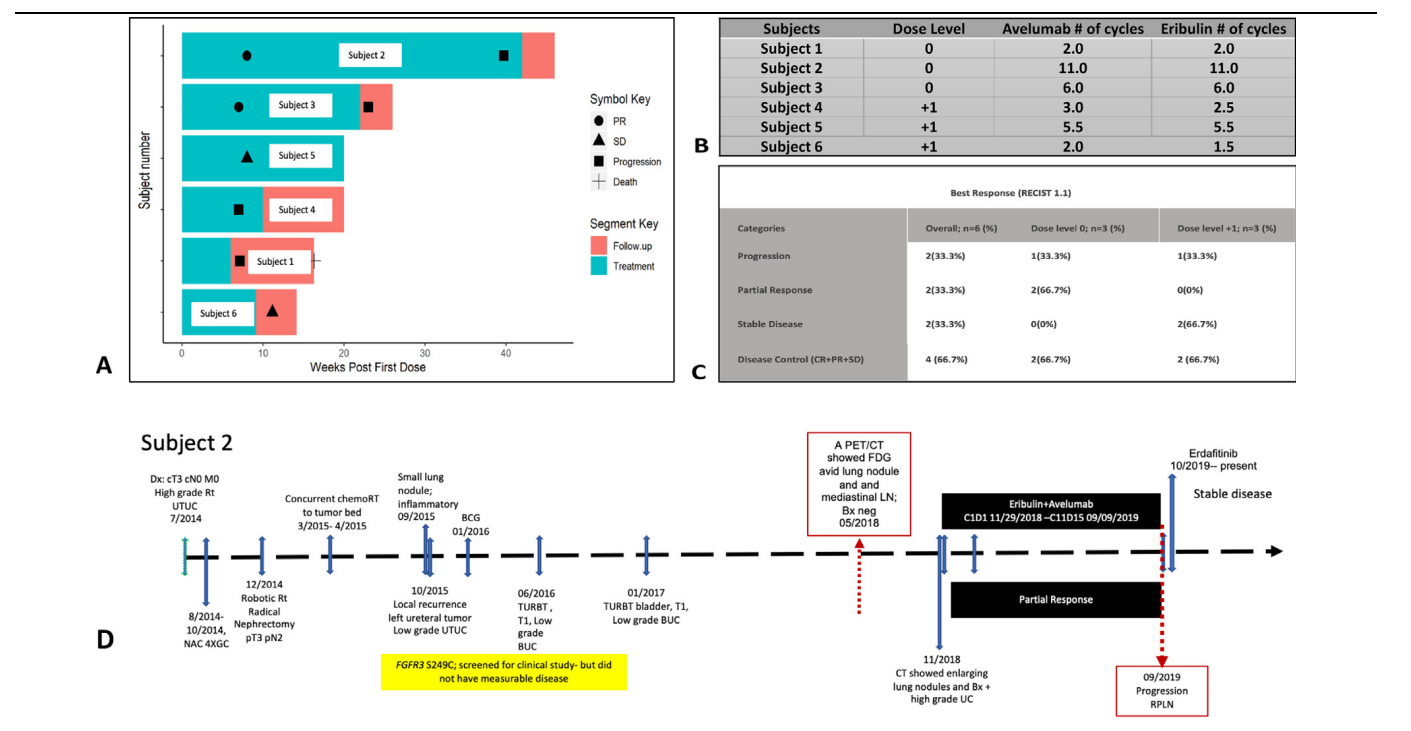
Avelumab和甲磺酸艾日不林(eribulin)在所有患者中的疗效
最后,研究人员指出,虽然这项试验的早期终止排除了任何明确的结论,但艾日布林和阿维单抗的联合治疗在mUC中显示出了前景。他们观察到,在较低剂量的艾日布林下,治疗的耐受性和有效性更好。该药物联用在mUC中的应用还需进一步研究。
原始出处:
Monika Joshi , Sheldon L Holder , Junjia Zhu et al. Avelumab in Combination with Eribulin Mesylate in Metastatic Urothelial Carcinoma: BTCRC GU-051, a Phase 1b Study. Eur Urol Focus. Mar 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#艾日布林#
30
#mAb#
29
#avelumab#
28
#转移性#
34